Chapter: Medicine Study Notes : Paediatrics
History Outline - Paediatrics
History Outline
·
General data: name, DOB,
Ethnicity, where they live
·
Presenting Complaint
·
History of presenting complaint:
o Chronological and including symptoms across all systems
o Treatments so far
o Contact history
o Family history of the complaint
·
Paediatric Past Medical History:
o Antenatal
o Birth/perinatal: Gestation, delivery, weight, APGARS, any special care, complications
o Feeding (breast, formula, solids) – detailed if relevant (eg which
formula, how much, which solids, how
much)
o Weight – growth history, where relevant growth and puberty in family
members
o Immunisations
· Milestones – including relevant milestones for the child now: Cover Gross and Fine motor, receptive and expressive language, social, play and self care skills.
o Past medical history
o Social/school
·
Medications
·
Allergies
·
Family History: ages and health
of parents and grandparents. Ages, names
and health of siblings
·
Social History:
o Parent‟s occupations
o Who cares for the child
o Schooling/childcare, performance at school
o Behaviour at home/school
o Sleeping arrangements and home circumstances
o Financial circumstances
o Alcohol, smoking
o Pets
o Problems/stresses at home
·
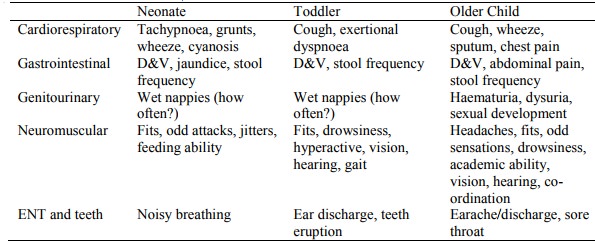
Systems enquiry
·
General questions: fatigue,
lumps, itch, fevers, bleeding tendency, family interaction
Related Topics