Chapter: Medicine Study Notes : Paediatrics
Asthma in Young Children
Asthma in Young Children
·
especially for Medication and
Spacer Use
·
3rd most common reason for admission
(after Bronchiolitis and URTI/Otitis media).
· Much much less common in < 1 years (NB bronchiolitis causes wheezing in young). Peak in 2 – 4 years
· Peak flow very unreliable under age 7 (and most bad asthmatics diagnosed from 2 – 5) ® have to rely on history
· History:
o Symptoms: waking at night with cough/wheeze, after exercise, how often
are attacks, had time off school/kindy as a result, how long does preventer
last
o Environmental factors: smokers, pets, damp, obvious triggers
o Current treatment: medicines, do the family understand the difference
between reliever and preventer, assess technique and compliance, is spacer
accepted by child and is it washed
· 2 patterns on history:
o Episodic (intermittent): viral URTI ® cough and wheeze. No interval symptoms
o Persistent (with exacerbations): interval symptoms (with exercise, at
night), exacerbations with viral infection, interferes with everyday life
·
Symptoms in a toddler:
o Cough, often worse at night
o May vomit with cough (NB exclude pertussis: cough ® choke ® vomit ® OK for an hour. In asthma, cough again straight away)
o Usually wheezy with URT infection
o Diagnosis difficult in an infant unless recurrent, strong immediate
family history or evidence of atopy
·
Physical findings in a toddler:
o Often normal chest exam
o If severe chronic symptoms:
§ Hyperinflated chest ( AP diameter)
§ Harrison‟s sulcus: dip in chest wall where diaphragm attaches
§ Eczema
§ Reduced growth (if severe)
o Stethoscope can be confusing
· Diagnosis:
o Cough is very common in kids (8 – 10 per year). But more during the day
than at night. Won‟t slow them down when running
o Is it asthma, bronchitis, bronchiolitis?
o Trial of therapy (preventative as well as relievers) and review
·
Criteria for admission:
o Pulse rate > 1.5 * normal
o Respiratory rate > 70 minute
o Chest
movements
o Restlessness/apathy/CNS depression or cyanosis/pallor [signs of
exhaustion]
·
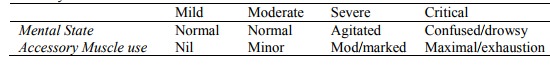
Severity assessment:
· Treatment:
o Avoid triggers: passive smoking, pets, house dust mite (dehumidifiers
don‟t work), pollens, cold, exercise, damp houses, certain foods (overstated)
o Infrequent episodic asthma:
§ Consider no therapy, avoid triggers
§ If distressed with attacks: use bronchodilators + spacer only. Start
during URTI phase. No preventative
o Frequent Episodic Asthma (only get it with a cold):
§ Intervals between attacks < 6 weeks
§ Bronchodilator as needed with URTIs
§ Prophylaxis:
§ Sodium cromoglycate (Vicrom + spacer).
?Evidence of poor efficacy
§ Nedocromil (Tilade + spacer)
§ Inhaled steroids: if it makes no difference then stop
·
Persistent Asthma
o Male: female = 4:1
o Preventative. If mild try Vicrom or Tilade. Moderate or severe use
inhaled steroids (takes 2 – 3 months for maximal effect). Titrate back once
controlled
o Bronchodilators as required
o Poor control: consider dose, check inhaler device and technique, poor compliance, environmental triggers
· Other treatment options:
o Long-acting b-agonists: salmeterol (Serevent), eformoterol (Foradil, Oxis)
o Theophylline (Nuelin, Theodur): 3rd line, gut ache ® poor compliance
o If severe: alternate day oral
prednisone treatment – reduced side effects (short and fat), and reasonable
asthma control
·
Protocol for an acute attack:
o Salbutamol dose: up to 5 years: 6 puffs via space. Over age 5: 12 puffs via space
o For severe add ipratropium (Atrovent)
o For moderate and severe, give doses at 0, 20, 40 and 60 minutes and review at 75 minutes
o Oral Steroid for all except minor attacks: 1 mg/Kg/day ® ¯relapse
Related Topics