Chapter: Medicine Study Notes : Paediatrics
Assessing Fluid State - Paediatrics Emergency Management
Emergency Management
Assessing Fluid State
Assessing Vital Signs
·
Rate is always subservient to
quality:
o Thready pulse: eg palpable at neck and groin only
o Respiration: more important that rate are grunting, flaring, subcostal
retraction, use of accessory muscles (in neonate ® bobbing
of head)
·
Blood volume:
·
Neonate 90 ml/kg
·
Child 80
ml/kg
·
Adult 70
ml/kg
o In a trauma situation, guess the weight: (age + 4) * 2
·
Urine output:
o In nappies: 2 ml/kg/hr
o Toilet trained: 1 ml/kg/hr
·
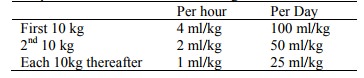
Normal fluid requirements in
absence of sweating:
·
Nutrition: to maintain weight
need 75 calories/kg/day
·
Heat loss:
o 70 kg person: surface to mass ratio is 0.02
o 2 kg person: surface to mass ratio is 0.08
o Rate of heat loss is proportional to (body temp – room temp) to the
power of 4. Best way to maintain body heat is therefore to heat the room.
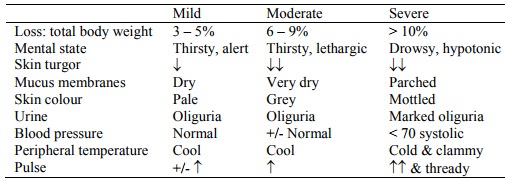
Assessing fluid loss
·
Only reliable indicator is
pulse. BP doesn‟t drop till severe
dehydration (compared with adult where
·
BP declines proportionately with
losses)
·
No physical signs until > 3%
loss
·
Most signs of dehydration are
those of shock
·
Change in body weight is the most
accurate estimate of fluid loss – but is rarely available
·
Dehydration in obese children is
often under-estimated
·
Nutrition: to maintain weight
need 75 calories/kg/day
·
Heat loss:
o 70 kg person: surface to mass ratio is 0.02
o 2 kg person: surface to mass ratio is 0.08
o Rate of heat loss is proportional to (body temp – room temp) to the
power of 4. Best way to maintain body heat is therefore to heat the room.
Assessing fluid loss
·
Only reliable indicator is pulse. BP doesn‟t drop till severe dehydration
(compared with adult where
·
BP declines proportionately with
losses)
·
No physical signs until > 3%
loss
·
Most signs of dehydration are
those of shock
·
Change in body weight is the most
accurate estimate of fluid loss – but is rarely available
·
Dehydration in obese children is
often under-estimated
·
Assessing turgor: pinched edge of
skin goes down slowly. Do centrally on
abdomen, chest, thighs
· Also when severe: rapid, sighing respirations (Kussmaul breathing)
·
Poor predictors of dehydration:
Sunken eyes or anterior fontanelle, dry mucous membranes, absence of sweat or
tears
Management of Non-Dehydrated Child
·
If no or infrequent vomiting that
is not interfering with fluid intake then 5 – 7 ml/kg/hour of:
o Breast milk
o ½ strength formula
o Fruit juice 1 part in 4 with water
·
After 6 – 12 hours introduce:
bananas, rice, potato, parsnips, pumpkin, dry biscuits/toast with vegemite
Management of Mild-Moderate Dehydration
·
Admit or observe in a short stay
facility for several hours
·
Don‟t use homemade solutions –
use Gastrolyte
· Orally, of by NG tube if necessary:
o Replace calculated losses over 6 hours (don‟t worry about maintenance
requirements). Hourly observations and reassess and reweigh after 6 hours
o Give the remainder of the daily fluid maintenance over the next 18 hours
·
Resume breast feeding as soon as
rehydration is complete or sooner if this takes longer than 6-hours
·
If after 4 – 6 hours the child
remains dehydrated, then IV
Management of Severe Rehydration
·
WEIGH THE CHILD to assess
progress
· 3 stages:
o Initial bolus if necessary. 10 - 20 ml/kg of Ringers Lactate or normal
saline over 10 – 15 minutes, reassess and repeat if necessary
o Replacement + maintenance
o Maintenance only
·
Rehydration of isotonic
dehydration:
o Replacement: Normal saline (or Ringer‟s Lactate or Hartmanns – more physiological)
o Maintenance: 1/5th normal saline + 5% Dextrose + 20 mmol/l KCl [Barts] (gives a bit much Cl
but the kidneys can sort that)
o If initially shocked, do not add KCl until urine is passed. If they have ATN following shock (® renal failure) don‟t want to overload K
· Timing:
o Infuse replacement fluid over 24 hours with the first 24 hours of
maintenance using ongoing replacement: ½ normal saline + 2.5%
dextrose + 10 mmol KCL (in 500 ml)
o Monitor electrolytes before, and during, up to 6 hourly
o Once they are able to tolerate oral fluids, treat as for mild/moderate
dehydration
·
Theme and variations:
o Diarrhoea:
§ Lost Na, HCO3, Cl and K from GI mucosal cells – replace
slowly
§ Resuscitation with bolus of crystalloids, eg Ringer‟s lactate, normal
saline
§ Maintenance with: ½ normal saline + 2.5% dextrose + 20 mmol/L KCL
§ If persistent acidosis due to HCO3 loss or lactic acidosis
then add in HCO3
o Rehydration of hypernatraemic dehydration (eg serum Na > 150):
§ Often the result of administering hyper-osmolar fluids (eg sports drinks) with vomiting and diarrhoea ® greater water loss due to water sucked into GI from circulation then vomited/passed
§ Will be more dehydrated than they appear due to fluid shifts from ICF ® ECF
§ If shocked give 10 ml/kg boluses of normal saline until circulation
restored
§ Calculate deficit
§ Calculate ongoing requirements over
48 hours
§ Give both over 48 hours –
serum sodium should not fall faster than 0.5 mmol/hr
§ If oral rehydration, replacement is over 24 hours
o Diabetic ketoacidosis:
§ If give insulin too fast, serum glucose will drop quickly ® rapid change in ECF osmolality ® cerebral oedema
§ If giving hypotonic solution then cerebral oedema – go slow
o Rehydration of hyponatraemic
dehydration (serum Na < 130):
§ Resulting from gut or renal losses, or excessive hypotonic fluid administration
§ Appear more dehydrated than they are as fluid shifts into the ICF. Can ® cerebral oedema, seizures, etc
§ Never give 1/5th normal saline (except to keep vein open). Do serial Na measurements
§ If asymptomatic: As for rehydration of isotonic dehydration, over 24 hours. Fluid restrict to 50% of maintenance
§ If symptomatic (seizures, coma) or if severe (Na < 120) then give 5 –
10 ml/kg or 3% hypertonic saline IV over 60 – 120 minutes in addition to the
calculated fluid requirements
·
Notes:
o Be careful about measuring volume: never hang a bag straight into a child
o If lung or brain disease (eg meningitis), SIADH is common Þ may need to fluid restrict (eg to 50% maintenance fluids). Check serum Na regularly
o In a term baby, born water logged (ECF > ICF). Can pass 500 ml urine
per day (7 ml/kg/hour). Handles water well but not used to passing a NaCl load
o Enemas for constipation can ® dehydration
Related Topics