Chapter: Medicine Study Notes : Paediatrics
Growth - Paediatrics
Growth
· Growth velocity = change in height over time. Declines till about 4, levels out, spike at puberty then zero
·
Factors influencing growth:
o Genetic potential
o Psychosocial factors (eg psychosocial dwarfism)
o Nutrition (including in utero): adequate calories, balance of nutrition
o Diseases in major systems: uses energy (eg
respiratory effort) and nutritional effects (eg GI)
o Hormones and Growth factors
·
Measurement:
o Method: Use stadiometer, fixed to wall, feet together, knees straight,
lift mastoid processes
o Accuracy and reliability:
§ SD of a single measurement ~ 0.25 cm. In a 5 year old this can cause a range in growth velocity from 10th to 50th centile
§ Taller in morning than at night
o Minimising error: Same measurer, calibrate regularly, careful
measurement, don‟t look at last measurement, measure at beginning and at end of
exam
Short Stature
·
Definition:
o > 2 standard deviations below the mean = below 5th centile
o Reduced growth velocity
·
Exclude failure to thrive
·
Growth pattern is more important
than height
·
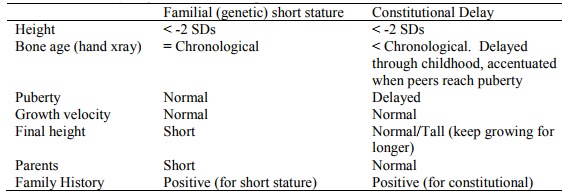
Normal variants:
o Familial (genetic) short stature
o Constitutional delay of growth and development. Presents mid to late childhood
·
Pathological causes:
o Systems: eg subclinical GI or renal disease (reflux, coeliac,
malabsorption, CF, etc)
o Psychosocial
o Genes:
§ Turner syndrome: webbed neck, wide nipples, wide carrying angle
§ Skeletal dysplasia: eg achondroplasia
§ Syndromes
o Hormones: Thyroid or GH deficiency, glucocorticoid excess
o Drugs: Steroids
·
Assessment:
o History:
§ Height: measured accurately and over time
§ Mid-parental height: assessment of genetic potential (adjusted so both parents are same sex as child. Male = female + 13 cm or average their centiles)
§ Family history: eg constitutional delay
§ Systems
§ Psychosocial
§ Development
o Examination:
§ Growth parameters
§ Dysmorphic features ® ?syndrome
§ Proportions: limbs vs trunk, eg arm span vs height, or upper segment
(head to pubic bone) vs lower segment (pubic bone to floor)
§ Blood pressure (?renal disease)
§ Fundi and visual fields (?pituitary tumour)
§ General
o Investigations:
§ Bone age: accurate to about 3 months
§ Specific depending on history/exam, eg renal ®
creatinine, coeliac ® antibodies
§ Karyotype in girls
·
Treatment:
o Treat cause
o Growth hormone:
§ Effective in GH deficiency and Turner‟s syndrome
§ May help in chronic renal failure, intrauterine growth retardation and
severe idiopathic short stature
o Androgens: consider in constitutional delay – won‟t influence final
height but get there faster.
Tall Stature
·
Arbitrary definition
·
Associated stigma (females more
often seek help)
·
Causes:
o Familial/genetic
o Over-nutrition
o Syndromes (eg XXY, Marfan‟s, Homocystinuria)
o Precocious puberty (tall early, but stop growing ®
eventually short)
o Growth hormone excess is extremely rare
Growing Pains *
· Occurs frequently: 15% of children with peak age of 11
·
Diagnosis of exclusion – no
organic pathology usually found. ?Child more vulnerable to pain and
stress-induced exacerbations
·
Occurs at least monthly for a
three-month period. Between times the
child is well
·
Differential:
o Orthopaedic disorders
o Collagen vascular disease
o Infection
o Neoplastic disorders
·
Management:
o Reassure, even if you can‟t find a cause
o Symptom diary (also check for psycho-social stressors)
o Symptomatic relief
Related Topics