Chapter: Medicine Study Notes : Paediatrics
Child Development
Growth and Development
Child Development
·
Represents the interaction of
heredity and the environment:
o Heredity: potential of the child
o Environment: extent to which potential is achieved. Requires:
·
Physical needs: warmth, clothing,
shelter, food, health, activity with rest
§ Psychological needs: security, personal identity, self-respect,
independence, opportunity to learn, play, affection and care
·
Areas of child development:
o Gross motor
o Find motor
o Language (expressive, receptive, non-verbal)
o Social (interaction, play, self-care)
o Cognitive: all of the above
·
Requirements for development
(need all of them):
o Hardware (neurons, muscles, etc)
o Motivation (often driven by frustration – a child can‟t do what it wants
to)
o Nurturing environment
·
Types of assessment:
o Developmental screening: point in time snapshot
o Developmental surveillance: following over time
o A formal assessment will yield a Developmental Quotient. < 100 Þ delay. 100 Þ advanced.
Developmental assessment
· Indirect assessment of the acquisition of life skills
·
Establish rapport: use names a
lot, „thanks for coming‟, etc ® more valid assessment
·
History:
o Current development and time course of development
o Order of questions should be:
§ When asking about milestones, start with things he is likely to be able
to do and work up. Get better rapport than starting at the upper limit and
working down
§ Hearing: What things can he hear?
·
Have you been concerned about his
hearing?
·
What makes you confident of that?
§ Vision: What small things does he see?
·
Have you been concerned?
· What makes you confident of that?
§ Gross motor: roll, sit, crawl, pull to stand, walk, run, scoot, pedal (progression: head ® trunk ® limbs)
§ Fine motor: pincer, feeding self, spoon, drawing, blocks
§ Expressive language: coo, babble, words with meaning, combinations (most common area of delay – usually focal not global)
§ Receptive language: Responds to familiar voice, to own name, one or two
step instruction, knows name, gender, address, prepositions, pronouns
§ Social: smile responsively, laugh, stranger aware, play with peers, name
friend
§ Self care: manage cup, spoon, undress, toilet, dress, laces
o Get history of influences on development:
§ Miscarriages, still births
§ Pregnancy: toxins, alcohol, infections
§ Birth: APGAR (usually means brain was vulnerable before birth),
gestation, birthweight
§ Neonatal congential abnormalities, feeding, jaundice, infections
§ Early milestones (smiling, sitting, walking, first words)
§ Illness (eg CF, heart/renal disease, epilepsy)
§ Hearing (®speech delay), vision (® good verbal, poor motor)
§ Nutrition, constipation (especially if mobility problems)
§ Current development, especially social, self-care
§ Behaviour problems (sleep, tantrums)
§ Family stress
§ Family history, especially of development
o History from other sources (eg kindy teacher)
o Review previous rate of development: may get slowing before loss
o Past Medical History: ABFWIMPS
·
Observation: Look systematically across each
of the 6 areas. Use toys as tools.
·
Examination:
o On lap first (stranger shyness from 8 months)
o Dysmorphism: eyes, head shape, body proportions
o Height, weight, head circumference – plot them
o Vision (do first, affects motor): following, hundreds and thousands
o Localise to noise (do before language): if concerned then formal testing
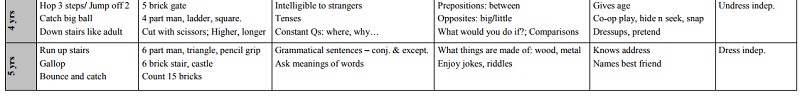
o For each of gross motor, fine motor, expressive and receptive language, social and self care on the table below:
§ Ask open-ended questions to establish the floor (eg I notice he‟s
walking, what other clever things is he doing)
§ Then use closed questions to establish a ceiling (eg can he walk backwards, throw over arm)
§ Then summarise: So he can ….. but is not yet …. Have I got that right?…
Therefore he is at age X for that domain
o Summary: age for each domain is X, Y, X.
Therefore, overall, he‟s developmentally around age
o [Average for X, Y, Z]
o Other:
§ Skin pigmentation (eg tuberous sclerosis – seen under Woods lamp)
§ Ears, eyes, heart, abdomen, puberty
§ Neurologic exam
§ Relationship with parents
·
Plan: for areas of weakness
o If significant delay then early intervention
o If some delay then anticipatory guidance – „what could you do to help‟ –
use Knowledge, attitudes/fears, practices, barriers framework
o Always pitch safety advice at the level of gross motor skills
Development Chart: normal development from 0-60 months
·
Ref: Dr Russell Wills
·
Red flags:
o Not smiling by 2 months
o No eye contact by 3 months
o Not reaching for objects by 5 months
o Not sitting unaided by 9 months
o Not walking unaided by 18 months
o Not using words by 18 months
o No 2 – 3 word sentences by 30/12 months

·
Older kids:
o Gross motor: bike (can ride without trainer wheels at 5), sport
(running, kicking), clumsiness
o Fine motor: computer, play station
o Cognitive: don‟t ask if does OK at school – everyone does OK these days!
Instead, does he do age appropriate work, need extra tuition, etc
Cognitive Development
· Overall process:
o Autonomy: dependent on parents ® peers ®
independent
o Abstract thinking (what if?): concrete ® mature
o Future consequences of present actions
o Gratification: immediate ® delayed
o Satisfaction with body image
o Black and white ® comfort with shades of grey
·
Infancy (birth – 2 years):
Developmental issues:
o Later develop goal directed activity
o Learn to distinguish between self and surroundings
o Develop object permanence
o Need secure attachment relationship with parents
o Separation, individuation in toddler years
o At 2: trial and error problem solving, planned and purposeful play but limited content, egocentric, parallel play
·
Preoperational (3 – 5 years):
o Egocentric world view (I made it happen, so it‟s my fault)
o Use of magical thinking, difficulty distinguishing real from symbolic
(if I wish it, it will come true)
o Trial and error problem solving only
o One aspect of a problem at a time
o Cannot order a series of events
o Cause and effect thinking: I did X, then Y happened, therefore X ® Y
o Imaginative play
o Gradually move from parallel play to interactive play with peers
o Separation and autonomy
o At 5: symbolic thought (imagination), classify by colour/shape, curiosity, magical thinking, social values, rules internalised but fixed, turn-taking, cooperative plan, other‟s perspective, increasing independence
·
Concrete Operational (6 - 10
years):
o Black and white thinking, right and wrong
o Capable of simple logic and problem solving
o Can order things in a chronological sequence
o May have difficulties with multiple perspectives
o Peer relationships increasingly important
o Sharing games, competition
o Analogy, metaphor, figures of speech being
o Able to concentrate for longer, delay gratification, predict personal
and social consequences of actions, plan ahead
·
Formal Operations (10 – 13
years):
o Better memory, concentration, forward planning
o Social skills refined
o Still concrete and literal (black/white, good/bad, right/wrong)
o Limited abstraction: eg what if I didn‟t do this? (Contrary-to-fact abstraction)
o Dramatic changes to body ® constant comparisons and normal
anxieties
o Need to conform with peer norms
o Difficult to take others perspective‟s
o Difficult to understand complexity
o Difficult to apply rules to own situation
o Lack future orientation/forward thinking
o Clear consequences
·
Middle Adolescence (14 – 16
years):
o Developing abstract and complex thought
o Beginning to see other‟s perspectives, starting to cope with shades of
grey
o Increased self consciousness
o Easily swayed – not certain of own view
o Still difficult to integrate conflicting ideas
o Narcissistic (feels good/what I want ® therefore its right ® impulsiveness)
o Less need to conform to peer norms, try alternative beliefs and
philosophies
o Need limits to be secure, limit testing
·
Late adolescence
o Adult memory and concentration
o Mature abstractions, problem-solving, self reflection and long range
planning
o Weigh up multiple information
o See multiple meanings, complex relationships, different points of view,
tolerant of shades of grey
o Able to think hypothetically and plan for possible events
o Remains more difficult to use new abilities in challenging situations
o Autonomous: able to leave home and return for counsel, rely on own
opinion
Developmental Delay
· Constant slow development leads to widening gap
·
Investigations: hearing, vision,
chromosomes, DNA screen (eg Fragile X, Angelman, Prader-Willi), thyroid, metabolic,
mucopolysaccharide screen, CK (Duchenne‟s), brain imaging, EEG
·
Type of Diagnosis:
o Functional Diagnosis:
§ Mobility, communication, learning, self-care, socialising, etc
§ What does the child need to achieve age-appropriate function
o Pattern diagnosis:
§ Autism
§ Cerebral palsy
§ Other syndromes
o Biological diagnoses: DNA disorders, brain injury
·
IQ scores:
o < 20 profound intellectual disability
o 20 – 35 severe
o 35 – 50 moderate
o 50 – 70 mild
o 70 – 85 borderline
o Definite or highly probable cause in majority < 50. Cause in about half < 70
·
Management:
o Objectives:
§ Maximising function
§ Preventing and treating secondary problems
§ Supporting carers
o Referral: paediatrician, geneticist, psychologist (eg cognitive
testing), SLT (speech, swallowing, play), physiotherapist (gross motor
problems), OT (fine motor, self care, aids and equipment), early intervention
groups, VNDT (Visiting Neurodevelopmental therapist), support groups
o Medical assessment of a diagnosed, disabled child
§ Always consider new illnesses
§ Look for syndrome specific health problems
§ Feeding difficulties, nutrition
§ Constipation
§ Medication
§ Carer Stress
§ Access to services and allowances
Tamariki Ora (Well Child) National Schedule
·
Covers:
o Health education and promotion
o Health protection and clinical assessment
o Family/whanau care and support
·
Health education/promotion topics
to cover at appropriate stages
·
Prevention:
o Types:
§ Primary: shifting the whole population curve ® improves
the overall standard
§ Secondary: identifying risk factors ® early or targeted intervention
§ Tertiary: minimising impact of established disease
o Benefits of prevention: ¯adult sequalae: injury, child abuse, delinquency and arrest rates
·
PPV of parental concerns about
delay is about 80 –90%. Must act or refer on parental concern
Related Topics