Chapter: Medicine Study Notes : Paediatrics
Congenital Heart Disease in Children
Congenital Heart Disease
Summary
· Congenital
o Acyanotic: Ventricular septal defect (VSD), Atrial septal defect (ASD), Atrioventricular Septal Defect (AVSD) and Patent ductus (PDA)
o Cyanotic:
§ Decreased Pulmonary Flow (® dark lungs on X-ray):
·
Critical pulmonary atresia/stenosis,
critical aortic stenosis (if not critical the acyanotic)
· Tricuspid atresia
·
Fallot‟s Tetralogy (commonest
congenital cyanotic problem, presents about 3 months of age, no murmur)
§ Increased pulmonary flow:
·
Transposition of the great
arteries (TGA): Fine till birth, goes blue as ductus closes
·
Total anomalous pulmonary venous
drainage (TAPVD): very rare
o Other: Coarctation
·
Acquired: Rheumatic fever
·
Arrhythmia: Long QT, SVT,
Pre-excitation, VT
·
If chronic leads to developmental
delay and clubbing
· Associated with:
o Chromosome disorders: Trisomy 21 (40% have cardiac lesion – mainly
AVSD), 18, 13 and Turners (coarctation)
o Numerous syndromes
Aetiology
· Genetic causes:
o 6 – 8/1000 live, full term births (higher in premature and still born).
Second most common congenital malformation after the brain
o Chromosomal eg Down Syndrome
o Single gene eg Marfan‟s (prolapsing mitral valve)
·
Environmental:
o Infection (eg Rubella)
o Maternal (eg Diabetes)
o Substance abuse (eg alcohol)
o Drugs (eg phenytoin, thalidamide)
·
Usually leads to an abnormality
in tissue migration
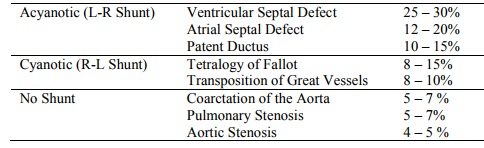
Incidence (Pathology not Paediatrics’ numbers!)
Ventricular Septal Defect
·
Epidemiology: 12/10,000
·
Types are muscular,
perimembranous and outlet (affects aortic valve)
·
90% involve membranous septum
which grows down to meet muscular wall
·
Clinical:
o Wide range: from asymptomatic through life to fulminant heart failure in
infancy
o Signs:
§ Pansystolic murmur (often with thrill)
§ Features of heart failure
§ Features of pulmonary hypertension if large: JVP,
sternal heave (RH work), loud P2
·
Investigations:
o ECG: LV hypertrophy (due to volume loading)
o CXR: heart size, vascular markings in lungs
o Echo: size and location of defect
·
Management: Treat only if large:
surgical repair
· Prognosis dependent on size of defect:
o Small defects often close over spontaneously. Remaining ones at risk of infective endocarditis. Prophylaxis if dental work.
o Large defects ® Eisenmenger‟s syndrome (see below, pulmonary hypertension, shunt reversal
and cyanosis)
Atrial Septal Defect (ASD)
·
Epidemiology: 6 – 8/10,000 live
full term births. F:M = 2:1. Higher in
stillborn and premature births
·
Aetiology unknown in > 90% of
cases
· Pathogenesis:
o Septum primum closes foramen primum at week 5. Failure to form completely results in a low ASD adjoining AV valve
o Septum secundum closes over foramen secundum at week 4 – flap forms a
one-way value. If it fails to reach far enough leads to fossa ovalis ASDs.
Common in trisomy 21
o Defects in primitive sinus venosus lead to ASD near vena cava ostia
· Clinical:
o A L ® R shunt increases pulmonary flow but if < 1 cm may be asymptomatic
through life
o Larger defects ® arrhythmias and/or murmur in 3rd decade. Evaluate for corrective surgery to prevent pulmonary hypertension, heart failure or arrhythmia
o Chronic pulmonary flow 2 – 4 times normal ® pulmonary hypertension with R ® L shunt and heart failure in less then 10% of cases
o Signs:
§ May have evidence of RH overload: JVP, sternal heave, loud P2
§ Ejection systolic murmur in pulmonary region (flow murmur due to flow, not due to defect). This is not specific – many children have it, especially when ill Þ P2 important in differentiating benign from ASD
§ Fixed splitting of S2
·
Investigations:
o ECG: RV hypertrophy and Right axis deviation (due to RV volume loading)
o CXR: heart size, prominent pulmonary artery with vascular
markings
o Echo to confirm diagnosis
·
Management: Surgical or
percutaneous closure by age 5 (unless small and spontaneous closure)
Patent Ductus Arteriosus
· Aetiology: Occurs as an isolated lesion or in combination with other abnormalities (eg Tetralogy of Fallot). Association with Rubella. 90% isolated defects. Incidence 1 in 2000
· Pathogenesis:
o Connects aorta to left pulmonary artery (acts as R ® L shunt in foetus).
o Oxygenation at birth ® ¯PGs (lungs metabolise them) ® muscular contraction ® functional closure at 2 days, anatomic closure at 2 – 3 months. Forms ligamentum arteriosum.
o If hypoxia at birth then it can remain patent. A patent ductus allows up to 75% of LV output to flow from the aorta to the pulmonary artery (ie becomes a L ® R shunt)
o If persistent then ® pulmonary hypertension ® becomes a R ® L shunt (Eisenmenger‟s Syndrome – see below), deoxygenated blood flows more to legs than arms ® clubbing in toes not fingers
· In term infants: Delayed closure due to ¯PaO2: pulmonary disease (eg meconium aspiration), pulmonary hypertension, high altitude
· In preterm:
o Incidence
with ¯ birth weight
o ¯ Sensitivity to PaO2 and sensitivity to PGE2
o Haemodynamic effect of hypoperfusion and hypotension: associated with
intraventricular haemorrhage and necrotising enterocolitis
·
Clinical:
o Murmur at left sternal edge, 2nd or 3rd intercostal space: systolic only. Silent if high pulmonary artery pressures (can be heard in first few hours in many infants)
o Active precordium with bounding pulses and pulse
pressure (collapsing pulse)
o Hepatomegaly
o LV failure: apnoea, bradycardia
o ® LV
hypertrophy, RV hypertrophy secondary to pulmonary hypertension if persistent
·
Investigations:
o ECG usually normal. LV and/or RV
hypertrophy if large and persistent
o CXR: cardiomegaly and pulmonary plethora
o Echo: diagnostic
·
Management:
o Requires closing:
§ NSAIDs (anti-PG) ® promote closure
§ Surgical or device closure
o Small risk of endocarditis if closed
Persistent Pulmonary Hypertension
· Failure of pulmonary capillary bed to dilate sufficiently after birth
·
Return to fetal circulation (ie R®L shunt):
¯ pulmonary flow
·
Causes:
o Aspiration, eg meconium
o Hypoxia: asphyxia
o Infection: Group B strep
o Hyaline membrane disease
o Lung hypoplasia
Coarctation of the Aorta
· Preductal or infantile form:
o Narrowing of the arch of the aorta between the left subclavian artery
and ductus arteriosus. Association with patent ductus and ASD (?due to low flow
in this area after birth) and with bicuspid aortic valves. Associated with
Turner‟s Syndrome. Severe consequences: LH failure, cyanosis in lower half of
body
o Variety of presentations:
§ Heart failure in infancy (LV hypertrophy due to pumping against an load)
§ Hypertension in child/young adult
§ Asymptomatic murmur
o Exam:
§ ¯Femoral
pulses, radio-femoral delay
§ Upper limb hypertension
§ Systolic murmur heard anteriorly and posteriorly (in back). Continuous murmur if severe
o Investigations:
§ ECG shows evidence of LV hypertrophy
§ CXR:
· Rib notching due to collaterals (> 5 years of age)
·
Abnormal aortic arch contour:
look for faint post stenotic dilatation below cardiac knuckle
§ Echo: shows lesion – harder to see descending aorta
§ Cardiac catheter: assess haemodynamics
o Treatment: surgery, balloon angioplasty and ongoing management (hypertension, risk of dissection, etc)
· Post ductal or adult form: Less severe narrowing with possible post-stenotic aneurysm due to turbulence. Ductus is closed. May be asymptomatic. Possible LV hypertrophy. Left intercostal artery provides collateral flow. (NB Proximal aneurysms occur in Syphilis, Coarctation and Marfan‟s)
·
Left and right pulses may be
different (left bounding)
Tetralogy of Fallot
·
Malformation during closure of
the interventricular septum leads to:
o Transposition/over-riding aorta
o High VSD
o Pulmonary valve stenosis/atresia
o Right ventricular hypertrophy (giving a boot shaped heart – diagnose on
X-ray)
·
Survival requires a patent ductus
·
Clinical: RH failure, commonly
endocarditis with subsequent brain abscess. Present several months after birth
with episodic blueness. Death likely at puberty if not corrected
Transposition of the Great Arteries (TGA)
·
Aortic and pulmonary arteries
transposed ® 2 separate circuits
·
Requires a patent ductus +/- VSD
·
OK until birth. Go blue as ductus closes
Pulmonary Valve Stenosis
· Similar effect to pulmonary atresia
·
® ¯ Right heart development. Blood has always got to LA via foramen ovale,
rather than through lungs
Other
·
Truncus arteriosus: congenital
malformation in which the pulmonary artery and aorta have failed to separate
from their common precursor truncus
Arrhythmias in Children
·
Relatively uncommon in paediatric
population
·
Often not associated with other
heart disease (cf adults, associated with structural disease)
·
Clinical
o Asymptomatic or palpitations
o If prolonged may ® growth retardation, heart failure, arrest, etc
·
Classification:
o Bradycardias:
§ AV Block:
·
1st and 2nd degree: normal variant
·
3rd degree: Associated with AVSD,
post-surgical, Rheumatic fever, myocarditis, maternal
§ mumps, etc. Acute treatment:
Isoprenaline/Atropine ® HR. Long term: pacemaker.
§ Sinus node dysfunction
o Tachycardias:
§ Supra-ventricular tachycardia (SVT): due to re-entrant pathway
associated with A-V node.
· Generally paroxysmal. Regular rhythm. Normal QRS duration. 1:1 A-V conduction.
· Management: Terminate tachycardia: vagal manoeuvres (ice on face, valsalva – breathing against closed glottis, carotid massage), IV adenosine (A-V node blocker), b-blockers, DC cardioversion. Prevent recurrences with b-blockers or ablation of re-entry pathway
§ Ventricular Tachycardias: rare in children. Cardiovert.
o Pre-excitation Syndromes: Wolfe-Parkinson White. Accessory pathway from atria to ventricle ® short PR interval, wide QRS and delta wave. Risk of cardiac arrest and sudden death. Treatment: ablation
o Long QT syndrome: due to congenital (K+ channel abnormality) or acquired
(drugs, hypocalcaemia). Susceptible to arrest, torsades and bradycardias.
Consider in unexplained syncope or convulsions. Treatment: cardiovert if
arrhythmia, b-blockers or pacemaker to prevent
Related Topics