Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Procuring Blood and Blood Products
Procuring Blood and Blood Products
BLOOD DONATION
To
protect both the donor and the recipients, all prospective donors are examined
and interviewed before they are allowed to donate their blood. The intent of
the interview is to assess the general health status of the donor and to
identify risk factors that might harm a recipient of the donor’s blood. Donors
should be in good health and without any of the following:
•
A history of viral hepatitis at any time in the
past, or a his-tory of close contact with a hepatitis or dialysis patient
within 6 months
•
A history of receiving a blood transfusion or an
infusion of any blood derivative (other than serum albumin) within 6 months
•
A history of untreated syphilis or malaria, because
these dis-eases can be transmitted by transfusion even years later. A person
who has been free of symptoms and off therapy for 3 years after malaria may be
a donor.
•
A history or evidence of drug abuse in which
substances were self-injected, because many intravenous/injection drug users
are hepatitis carriers and because the risk for human immunodeficiency virus
(HIV) is high in this group
•
A history of possible exposure to HIV; the
population at risk includes people who engage in anal sex, people with multiple
sexual partners, intravenous/injection drug users, sexual partners of people at
risk for HIV, and people with hemophilia
•
A skin infection, because of the possibility of
contami-nating the phlebotomy needle, and subsequently the blood itself
•
A history of recent asthma, urticaria, or allergy
to medica-tions, because hypersensitivity can be transferred passively to the
recipient
•
Pregnancy within 6 months, because of the
nutritional de-mands of pregnancy on the mother
•
A history of tooth extraction or oral surgery
within 72 hours, because such procedures are frequently associated with
tran-sient bacteremia
•
A history of exposure to infectious disease within
the past 3 weeks, because of the risk of transmission to the recipient
•
Recent immunizations, because of the risk of
transmitting live organisms (2-week waiting period for live, attenuated
organisms; 1 month for rubella; 1 year for rabies)
•
A history of recent tattoo, because of the risk of
blood-borne infections (eg, hepatitis, HIV)
•
Cancer, because of the uncertainty about
transmission of the disease
•
A history of whole blood donation within the past
56 days
Potential
donors should be asked whether they have consumed any aspirin or
aspirin-containing medications within the past 3 days. Although aspirin use does
not render the donor ineligible, the platelets obtained would be dysfunctional
and therefore not useful. Aspirin does not affect the RBCs or plasma obtained
from the donor.
All
donors are expected to meet the following minimal re-quirements:
•
Body weight should exceed 50 kg (110 pounds) for a
stan-dard 450-mL donation. Donors weighing less than 50 kg do-nate
proportionately less blood. People younger than 17 years of age are
disqualified from donation.
•
The oral temperature should not exceed 37.5°C (99.6°F).
•
The pulse rate should be regular and between 50 and
100 beats per minute.
•
The systolic arterial pressure should be 90 to 180
mm Hg, and the diastolic pressure should be 50 to 100 mm Hg.
•
The hemoglobin level should be at least 12.5 g/dL
for women and 13.5 g/dL for men.
Directed Donation
At
times, friends and family of a patient wish to donate blood for that person.
These blood donations are termed directed dona-tions. These donations are not
any safer than those provided by random donors, because directed donors may not
be as willing to identify themselves as having a history of any of the risk
factors that disqualify a person from donating blood.
Standard Donation
Phlebotomy
consists of venipuncture and blood withdrawal. Standard precautions are used.
Donors are placed in a semi-recumbent position. The skin over the antecubital
fossa is carefully cleansed with an antiseptic preparation, a tourniquet is
applied, and venipuncture is performed. Withdrawal of 450 mL of blood usually
takes less than 15 minutes. After the needle is removed, donors are asked to
hold the involved arm straight up, and firm pressure is applied with sterile
gauze for 2 or 3 minutes or until bleeding stops. A firm bandage is then
applied. Donors remain recumbent until they feel able to sit up, usually within
a few min-utes. Donors who experience weakness or faintness should rest for a
longer period. Donors then receive food and fluids and are asked to remain
another 15 minutes.
Donors
are instructed to leave the dressing on and to avoid heavy lifting for several
hours, to avoid smoking for 1 hour, to avoid drinking alcoholic beverages for 3
hours, to increase fluid intake for 2 days, and to eat a healthy meals for 2
weeks. Specimens from this donated blood are tested to detect in-fections and
to identify the specific blood type (see later discussion).
Autologous Donation
A
patient’s own blood may be collected for future transfusion; this method is
useful for many elective surgeries where the po-tential need for transfusion is
high (eg, orthopedic surgery). Pre-operative donations are ideally collected 4
to 6 weeks before surgery. Iron supplements are prescribed during this period
to prevent depletion of iron stores. Occasionally, erythropoietin (epoetin-alfa
[Epogen, Procrit]) is given to stimulate erythro-poiesis to ensure that the
donor’s hematocrit remains high enough to be eligible for donation. Typically,
1 unit of blood is drawn each week; the number of units obtained varies with
the type of surgical procedure to be performed (ie, the amount of blood
anticipated to be transfused). Phlebotomies are not per-formed within 72 hours
of surgery. Individual blood compo-nents can also be collected.
The
primary advantage of autologous transfusions is the pre-vention of viral infections
from another person’s blood. Other ad-vantages include safe transfusion for
patients with a history of transfusion reactions, prevention of
alloimmunization, and avoid-ance of complications in patients with
alloantibodies. The policy of the American Red Cross requires autologous blood
to be trans-fused only to the donor. If the blood is not required, it can be
frozen until the donor needs it in the future (for up to 10 years). The blood
is never returned to the general donor supply of blood products to be used by
someone else.
The
disadvantage of autologous donation is that it may be per-formed even when the
likelihood that the anticipated procedure will necessitate a transfusion is
small. Needless autologous dona-tion is expensive, takes time, and uses
resources inappropriately. Moreover, in an emergency situation, the autologous
units avail-able may be inadequate, and the patient may still require
additional units from the general donor supply.
Contraindications
to donation of blood for autologous transfusion are acute infection, severely
debilitating chronic disease, hemoglobin level less than 11 g/dL, hematocrit
less than 33%, unstable angina, and acute cardiovascular or cere-brovascular
disease. A history of poorly controlled epilepsy may be considered a
contraindication in some centers. Patients with cancer may donate for
themselves.
Intraoperative Blood Salvage
This
transfusion method provides replacement for patients who are unable to donate
before surgery and for those undergoing vas-cular, orthopedic, or thoracic
surgery. During a surgical proce-dure, blood lost into a sterile cavity (eg,
hip joint) is suctioned into a cell-saver machine. The RBCs are washed, often
with saline solution, and then returned to the patient as an intravenous in-fusion.
Salvaged blood cannot be stored, because bacteria cannot be completely removed
from the blood.
Hemodilution
This
transfusion method is initiated before or after induction of anesthesia. About
1 or 2 units of blood are removed from the pa-tient through a venous or
arterial line and simultaneously replaced with a colloid or crystalloid
solution. The blood obtained is then reinfused after surgery (Kreimeier &
Messmer, 2002). The advan-tage of this method is that the patient loses fewer
RBCs during surgery, because the added intravenous solutions dilute the
con-centration of RBCs and lower the hematocrit. Patients who are at risk for
myocardial injury, however, should not be further stressed by hemodilution.
COMPLICATIONS OF BLOOD DONATION
Excessive
bleeding at the donor’s venipuncture site is sometimes caused by a bleeding
disorder in the donor but more often results from a technique error: laceration
of the vein, excessive tourniquet pressure, or failure to apply enough pressure
after the needle is withdrawn.
Fainting
is common after blood donation and may be related to emotional factors, a
vasovagal reaction, or prolonged fasting be-fore donation. Because of the loss
of blood volume, hypotension and syncope may occur when the donor assumes an
erect position. A donor who appears pale or complains of faintness should
im-mediately lie down or sit with head lowered below the knees; he or she
should be observed for another 30 minutes.
Anginal
chest pain may be precipitated in patients with un-suspected coronary artery
disease. Seizures can occur in donors with epilepsy, although the incidence is
very low. Both angina and seizures require further medical evaluation.
Many
people have the misconception that donating blood can cause AIDS and other
infections. Potential donors need to be ed-ucated that the equipment used in
donation is sterile, a closed sys-tem, and not reusable; they are at no risk
for acquiring such infections from donating blood.
BLOOD PROCESSING
Samples
of the unit of blood are always taken immediately after donation so that the
blood can be typed and tested. Each do-nation is tested for antibodies to HIV 1
and 2, hepatitis B core antibody (anti-HBc), hepatitis C virus (HCV), and human
T-cell lymphotropic virus, type I (anti-HTLV-I/II). The blood is also tested
for hepatitis B surface antigen (HbsAG) and for syphilis. Negative reactions
are required for the blood to be used, and each unit of blood is labeled to
certify the results. A new testing method, using nucleic acid amplification testing
(NAT), has increased the ability to detect the presence of HCV and HIV
infection, because it directly tests for genomic nucleic acids of the virus
itself, rather than for the presence of antibodies to the virus (Korman, Leparc
& Benson, 2001). This testing significantly shortens the “window” of
inability to detect HIV and HCV from a donated unit, further ensuring the
safety of the blood. Blood is also screened for CMV; if it tests positive for
CMV, it can still be used, except in recipients who are neg-ative for CMV and
who are immunocompromised (eg, BMT or PBSCTrecipients).
Equally
important to viral testing is accurate determination of the blood type. More
than 200 antigens have been identified on the surface of RBC membranes. Of
these, the most important for safe transfusion are the ABO and Rh systems. The
ABO system identifies which sugars are present on the membrane of an
indi-vidual’s RBCs: A, B, both A and B, or neither A nor B (type O). To prevent
a significant reaction, the same type of RBCs should be transfused. Previously,
it was thought that in an emergency sit-uation in which the patient’s blood
type was not known, type O blood could be safely transfused. This practice is
no longer ad-vised by the American Red Cross.
The Rh
antigen (also called D) is present on the surface of RBCs in 85% of the
population (Rh-positive). Those who lack the D antigen are called Rh-negative.
RBCs are routinely tested for the D antigen as well as ABO. Patients should
receive PRBCs with a compatible Rh type.
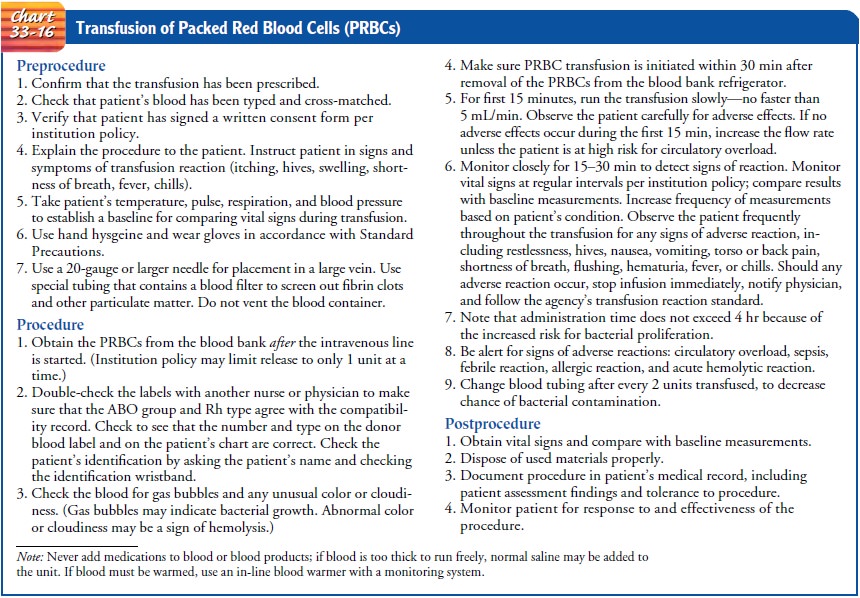
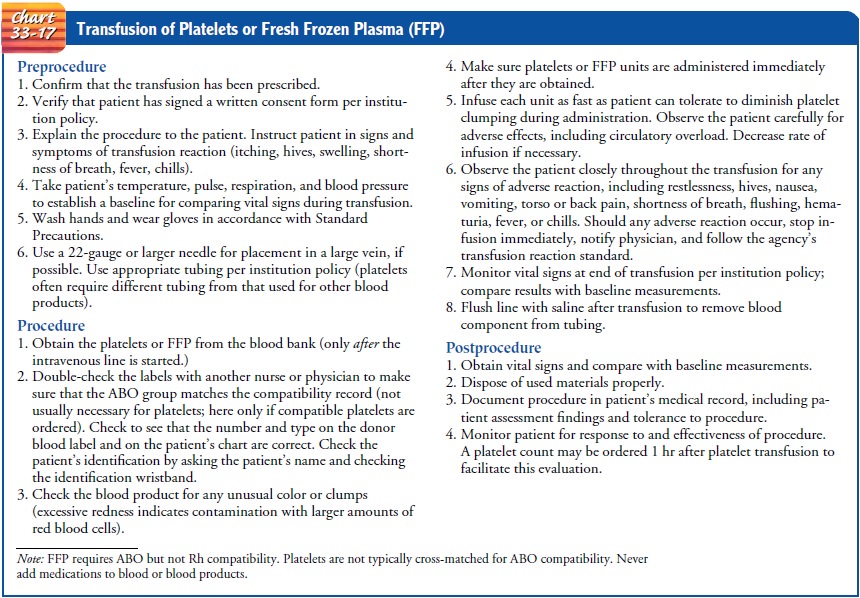
TRANSFUSION
Administration
of blood and blood components requires knowl-edge of correct administration
techniques and possible complica-tions. It is very important to be familiar
with the agency’s policies and procedures for transfusion therapy. Methods for
transfusing blood components are presented in Charts 33-16 and 33-17. Potential
complications of transfusion follow.
Setting
Although
most blood transfusions are performed in the acute care setting, patients with
chronic transfusion requirements often can receive transfusions in other
settings. Free-standing infusion cen-ters, ambulatory care clinics, a
physician’s office, and even the home may be appropriate settings for
transfusion. Typically, pa-tients who need chronic transfusions but are
otherwise stable physically are appropriate candidates for outpatient therapy.
Ver-ification and administration of the blood product are performed much as in
a hospital setting. Although most blood products can be transfused in the
outpatient setting, the home is typically lim-ited to transfusions of PRBCs and
factor components (eg, factor VIII for patients with hemophilia)
Pretransfusion Assessment
PATIENT HISTORY
Patient history is an important component of the pretransfu-sion assessment to determine the history of previous transfu-sions as well as previous reactions to transfusion. The history should include the type of reaction, its manifestations, the in-terventions required, and whether any preventive interventions were used in subsequent transfusions. It is important to assess the number of pregnancies a woman has had, because an in-creased number can increase her risk for reaction due to anti-bodies developed from exposure to fetal circulation. Other concurrent health problems should also be noted, with careful attention to cardiac, pulmonary, and vascular disease.
PHYSICAL ASSESSMENT
A
systematic physical assessment and measurement of baseline vital signs are
important before transfusing any blood product. The res-piratory system should
be assessed, including careful auscultation of the lungs and for use of
accessory muscles. Cardiac system as-sessment should include careful inspection
for any edema as well as other signs of cardiac failure (eg, jugular venous
distention). The skin should be observed for rashes, petechiae, and
ecchy-moses. The sclera should be examined for icterus. In the event of a
possible transfusion reaction, a comparison of findings can help differentiate
between types of reactions.
Patient Teaching
Reviewing
the signs and symptoms of a potential transfusion re-action is crucial for
patients who have not received a transfusion be-fore. Even for those patients
who have received prior transfusions, a brief review of signs and symptoms of
potential transfusion reac-tions is advised. Signs and symptoms of a possible
reaction include fever, chills, respiratory distress, low back pain, nausea,
pain at the intravenous site, or anything “unusual.” Although a thorough
re-view is very important, it is also important to reassure the patient that
the blood is carefully tested against the patient’s own blood (cross-matched)
to diminish the likelihood of any untoward reac-tion. Such assurance can be
extremely beneficial in allaying anxi-ety. Similarly, it can be useful to
mention again the very low possibility of contracting HIV from the transfusion;
this fear per-sists among many people.
Related Topics