Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Leukopenia and Neutropenia
Leukopenia and Neutropenia
Leukopenia,
a condition in which there are fewer WBCs than normal, results from neutropenia
(diminished neutrophils) or lym-phopenia (diminished lymphocytes). Even if
other types of WBCs (eg, monocytes, basophils) are diminished, their numbers
are too few to reduce the total WBC count significantly. Lymphopenia
(lymphocytes less than 1500/mm3) can result from ionizing radia-tion, long-term
use of corticosteroids, uremia, some neoplasms (eg, breast and lung cancers,
advanced Hodgkin’s disease), and some protein-losing enteropathies (in which
the lymphocytes within the intestines are lost).
NEUTROPENIA
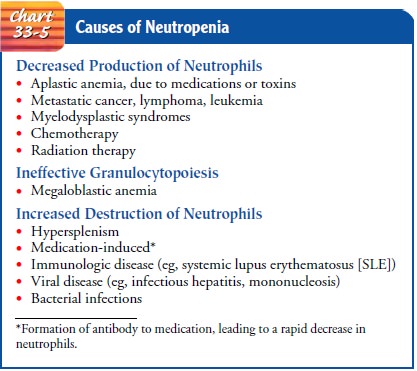
Neutropenia (neutrophils less than 2000/mm3) results from de-creased production of neutrophils or increased destruction of these cells (Chart 33-5). Neutrophils are essential in preventing and lim-iting bacterial infection. A patient with neutropenia is at increased risk for infection, both exogenous and endogenous (the gastro intestinal tract and skin are common endogenous sources).
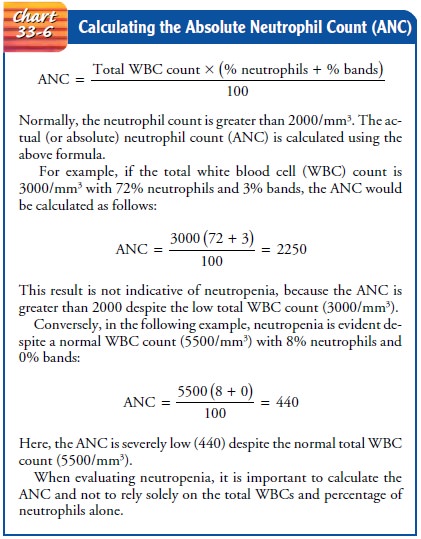
The risk for infection is based not only on the severity of the neu-tropenia (low neutrophil count), but also on the duration of the neutropenia. The actual number of neutrophils, known as the ab-solute neutrophil count (ANC), is determined by a simple math-ematical calculation using data obtained from the CBC and differential test (Chart 33-6). The risk of infection increases pro-portionately with the decrease in neutrophil count. The risk is sig-nificant when the ANC is less than 1000, is high when it is less than 500, and is almost certain when it is less than 100.
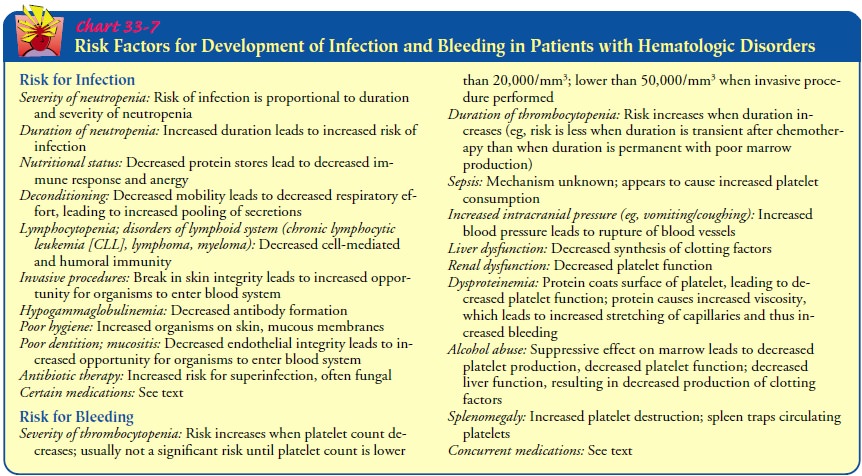
The risk of
developing infection increases with the length of time during which neutropenia
persists, even if it is fairly mild. Conversely, even a severe neutropenia may
not result in infection if the dura-tion of the neutropenia is brief, as is
often seen after chemotherapy (Chart 33-7).
Clinical Manifestations
There
are no definite symptoms of neutropenia until the patient becomes infected.
Routine CBC with differential tests, such as those obtained after chemotherapy
treatment, can reveal neu-tropenia before the onset of infection.
Medical Management
Treatment
of the neutropenia varies depending on its cause. If the neutropenia is
medication induced, the offending agent needs to be stopped, if possible.
Treatment of an underlying neoplasm can temporarily make the neutropenia worse,
but with bone mar-row recovery treatment may improve it. Corticosteroids may be
used if the cause is an immunologic disorder. The use of growth fac-tors such
as G-CSF or granulocyte/macrophage colony-stimulating factor (GM-CSF) can be
effective in increasing neutrophil pro-duction when the cause of the neutropenia
is decreased produc-tion. Withholding or reducing the dose of chemotherapy or
radiation therapy may be required when the neutropenia is caused by these
treatments; however, in the case of potentially curative therapy,
administration of growth factor is considered to be prefer-able, so that the
maximum antitumor effect can be achieved. Should the neutropenia be accompanied
by fever, the patient is automatically considered to be infected and usually is
admitted to the hospital. Cultures of blood, urine, and sputum should be
ob-tained, as well as a chest radiograph. To ensure adequate therapyagainst the
invading infectious organisms, broad-spectrum antibi-otics are initiated as
soon as the samples for culture are obtained, although the medications may be
changed after culture and sensi-tivity results become available.
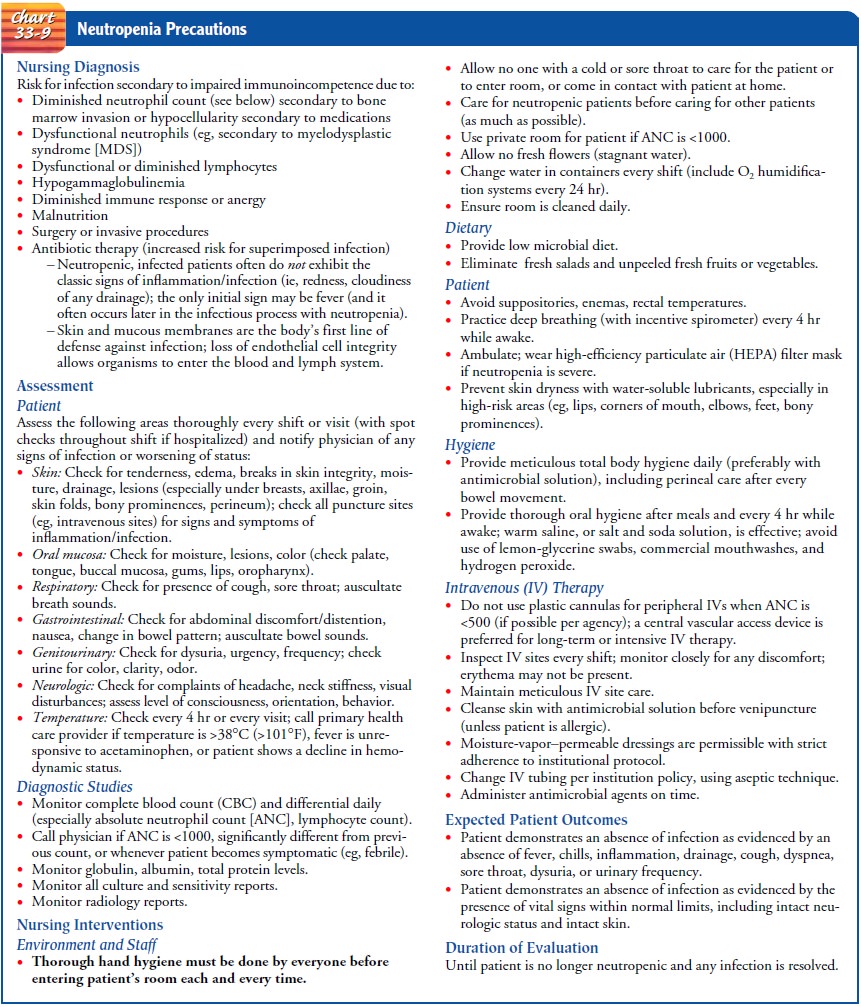
Nursing Management
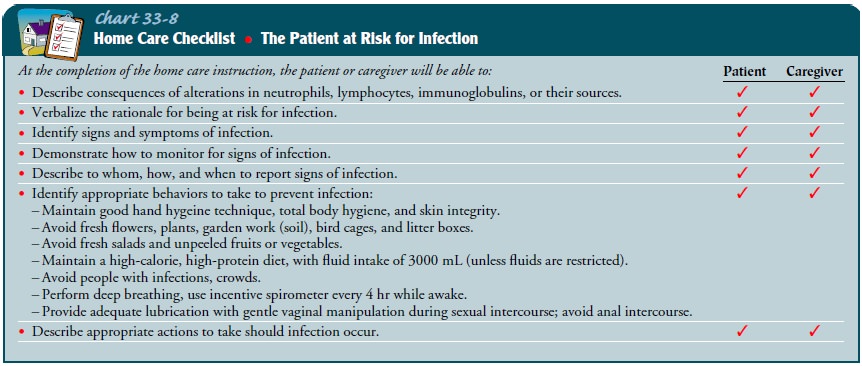
Nurses
in all settings have a crucial role in assessing the severity of neutropenia
and in preventing and managing infectious com-plications. Patient teaching is
equally important, particularly in the outpatient setting, so that the patient
can implement appro-priate self-care measures and know when and how to seek
medical care (Chart 33-8). Patients at risk for neutropenia should have blood
drawn for CBCs; the frequency is based on the suspected severity and duration
of the neutropenia. Nurses need to be able to calculate the ANC (see Chart
33-6) and to assess the severity of neutropenia and the risk for infection.
Chart 33-9 identifies nursing interventions related to neutropenia.
Related Topics