Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Immune Hemolytic Anemia
IMMUNE
HEMOLYTIC ANEMIA
Hemolytic
anemias can result from exposure of the RBC to anti-bodies. Alloantibodies (ie,
antibodies against the host, or “self”) re-sult from the immunization of an
individual with foreign antigens (eg, the immunization of an Rh-negative person
with Rh-positive blood). Alloantibodies tend to be large (IgM type) and cause
im-mediate destruction of the sensitized RBCs, either within the blood vessel
(intravascular hemolysis) or within the liver. The most com-mon type of
alloimmune hemolytic anemia in adults results from a hemolytic transfusion
reaction.
Autoantibodies
are developed by an individual for varying rea-sons. In many instances, the
person’s immune system is dysfunc-tional, so that it falsely recognizes its own
RBCs as foreign and produces antibodies against them. This mechanism is seen in
peo-ple with chronic lymphocytic leukemia (CLL). Another mecha-nism is a
deficiency in suppressor lymphocytes, which normally prevent antibody formation
against a person’s own antigens. Auto-antibodies tend to be of the IgG type.
The RBCs are sequestered in the spleen and destroyed by the macrophages outside
the blood vessel (extravascular hemolysis).
Autoimmune
hemolytic anemias can be classified based on the body temperature involved when
the antibodies react with the RBC antigen. Warm-body antibodies bind to RBCs
most actively in warm conditions (37°C);
cold-body antibodies react in cold (0°C).
Most autoimmune hemolytic anemias are the warm-body type. Autoimmune hemolytic
anemia is associated with other dis-orders in most cases (eg, medication
exposure, lymphoma, CLL, other malignancy, collagen vascular disease,
autoimmune disease, infection). In idiopathic autoimmune hemolytic states, the
reason why the immune system produces the antibodies is not known. All ages and
genders are equally vulnerable to this form, whereas the incidence of secondary
forms is greater in people older than 45 years of age and in females.
Clinical Manifestations
Clinical
manifestations can vary, and they usually reflect the degree of anemia. The
hemolysis may be very mild, so that the patient’s marrow compensates adequately
and the patient is asymptomatic. At the other extreme, the hemolysis can be so
severe that the resultant anemia is life-threatening. Most patients complain of
fatigue and dizziness. Splenomegaly is the most common physical finding,
occurring in more than 80% of patients; hepatomegaly, lym-phadenopathy, and
jaundice are also common.
Assessment and Diagnostic Findings
The
laboratory tests show a low hemoglobin level and hematocrit, most often with an
accompanying increase in the reticulocyte count. RBCs appear abnormal;
spherocytes are common. The serum bilirubin level is elevated, and if the
hemolysis is severe, the haptoglobin level is low or absent. The Coombs test (also
referred to as the direct antiglobulin test [DAT]), which detects antibodies on
the surface of RBCs, shows a positive result.
Medical Management
Any
possibly offending medication should be immediately dis-continued. The
treatment consists of high doses of corticosteroids (1 mg/kg per day) until
hemolysis decreases. Corticosteroids de-crease the macrophage’s ability to
clear the antibody-coated RBCs. If the hemoglobin level returns toward normal,
usually after sev-eral weeks, the corticosteroid dose can be lowered or, in
some cases, tapered and discontinued. However, corticosteroids rarely produce a
lasting remission. In severe cases, blood transfusions may be required. Because
the antibody may react with all possible donor cells, careful blood typing is
necessary, and the transfusion should be administered slowly and cautiously.
Splenectomy
(removal of the spleen) removes the major site of RBC destruction; therefore,
splenectomy may be performed if corticosteroids do not produce a remission. If
neither cortico-steroid therapy nor splenectomy is successful,
immunosuppressive agents may be administered. The two immunosuppressive agents
most frequently used are cyclophosphamide (eg, Cytoxan), which has a more rapid
effect but more toxicity, or azathioprine (Imu-ran), which has a less rapid
effect but less toxicity. The synthetic androgen danazol (Cyclomen, Danocrine)
can be useful in some patients, particularly in combination with
corticosteroids. The mechanism for this success is unclear. If corticosteroids
or im-munosuppressive agents are used, the taper must be very gradual to
prevent a rebound “hyperimmune” response and exacerbation of the hemolysis.
Immunoglobulin administration is effective in about one third of patients, but
the effect is transient and the med-ication is expensive. Transfusions may be
necessary if the anemia is severe; it may be extremely difficult to cross-match
samples of available units of RBCs with that of the patient.
For
patients with cold-antibody hemolytic anemia, treatment may not be required,
other than to advise the patient to keep warm; relocation to a warm climate may
be necessary.
Nursing Management
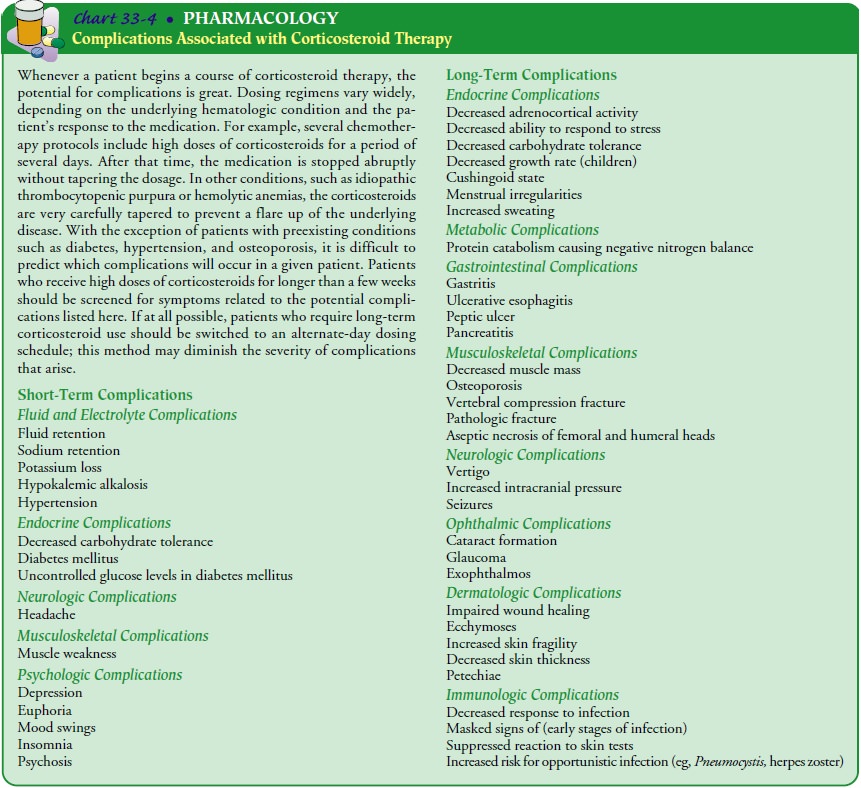
Patients
may have great difficulty understanding the pathologic mechanisms underlying
the disease and need repeated explana-tions in terms they can understand.
Patients who have had a splenectomy should be vaccinated against pneumococcal
infec-tions (Pneumovax) and informed that they are permanently at greater risk
for infection. Patients receiving long-term cortico-steroid therapy,
particularly those with concurrent diabetes or hy-pertension, need careful
monitoring. They must understand the need for this medication and the
importance of never abruptly dis-continuing it. A written explanation and a
tapering schedule should be provided, and adjustments based on hemoglobin
levels should be emphasized. Similar teaching should be provided when
immunosuppressive agents are used. Corticosteroid therapy is not without
significant risk, and patients need to be monitored closely for complications.
The short- and long-term complications of cor-ticosteroid therapy are presented
in Chart 33-4.
Related Topics