Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Pathophysiology of the Hematologic System
PATHOPHYSIOLOGY
OF THE HEMATOLOGIC SYSTEM
Most
hematologic diseases reflect a defect in the hematopoietic, he-mostatic, or RES
systems. The defect can be quantitative (eg, in-creased or decreased production
of cells), qualitative (eg, the cells that are produced are defective in their
normal functional capac-ity), or both.
Gerontologic Considerations
In
elderly patients, a common problem is decreased ability of the bone marrow to
respond to the body’s need for blood cells (RBCs, WBCs, and platelets). This
inability is a result of many factors, in-cluding diminished production of the
growth factors necessary for hematopoiesis by stromal cells within the marrow
or a diminished response to the growth factors (in the case of erythropoietin).
When an elderly person needs more blood cells (eg, WBCs in infection, RBCs in
anemia), the bone marrow may not be able to increase production of these cells
adequately.Leukopenia (a de-creased
number of circulating WBCs) or anemia can result. In the elderly, the bone
marrow may be more susceptible to the myelo-suppressive effects of medications.
Anemia
is the most common hematologic condition affecting elderly patients; with each
successive decade of life, the incidence of anemia increases. Anemia frequently
results from iron deficiency (in the case of blood loss) or from a nutritional
deficiency, partic-ularly folate or B12 deficiency or protein-calorie malnutrition;
it may also result from inflammation or chronic disease. Manage-ment of the
disorder varies depending on the etiology. Therefore, it is important to
identify the cause of the anemia rather than to consider it an inevitable
consequence of aging. Elderly people with concurrent cardiac or pulmonary
problems may not tolerate ane-mia very well, and a prompt, thorough evaluation
is warranted.
Assessment and Diagnostic Findings
Many
hematologic conditions cause few symptoms. Therefore, the use of extensive
laboratory tests is often required to diagnose a hematologic disorder. For most
hematologic conditions, contin-ued monitoring via specific blood tests is
required because it is very important to assess for changes in test results
over time.
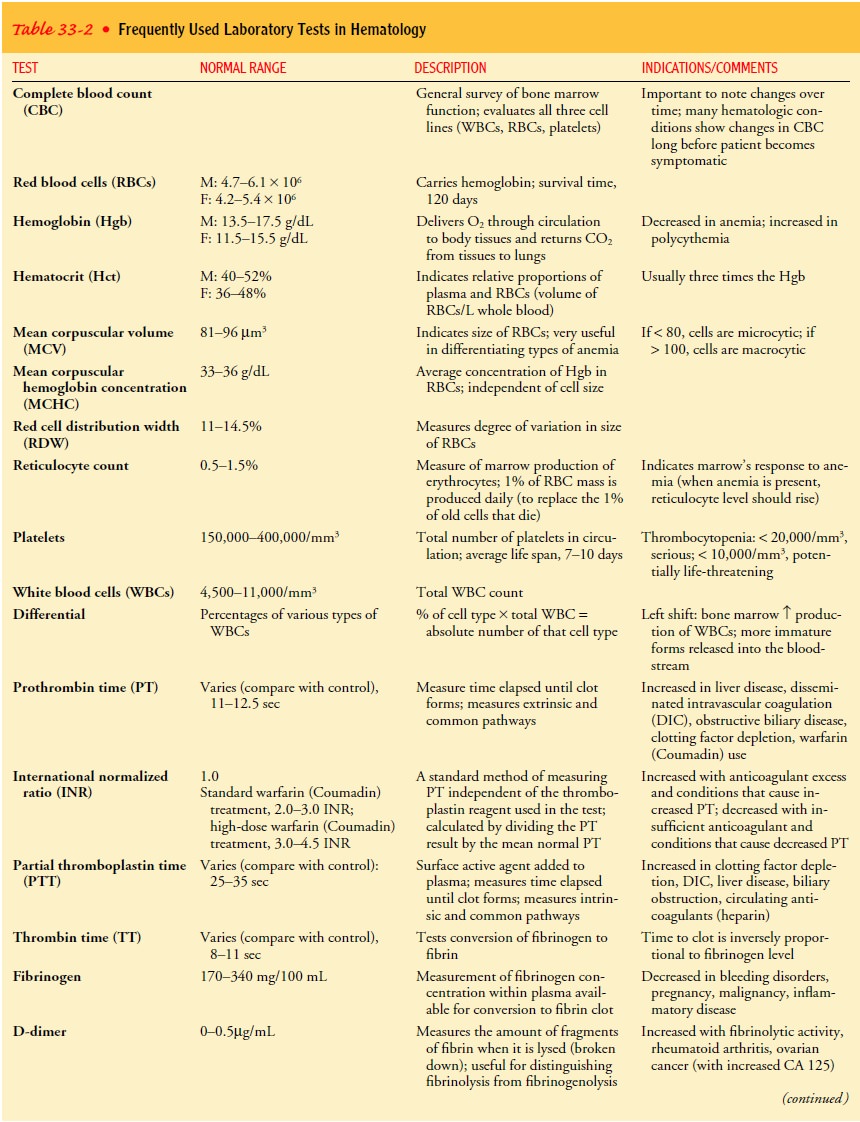
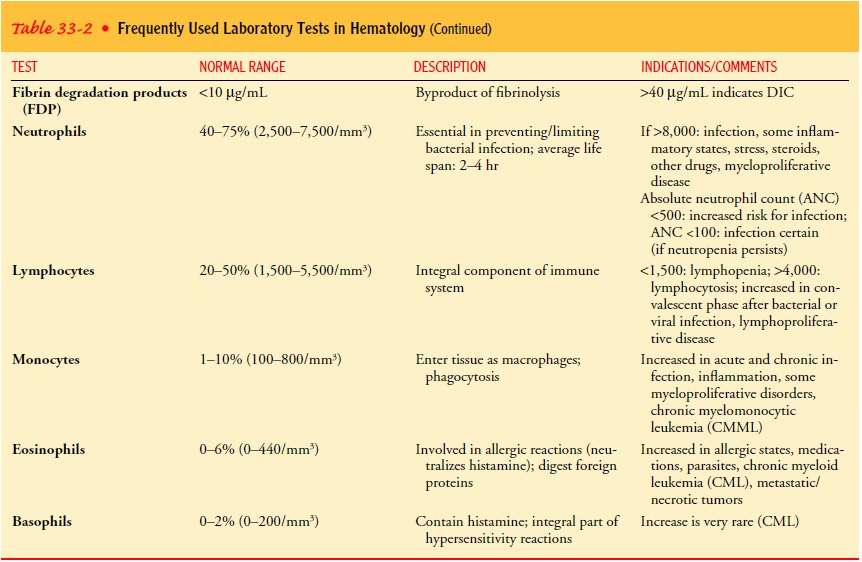
HEMATOLOGIC STUDIES
The
most common tests used are the complete blood count (CBC) and the peripheral
blood smear (Table 33-2). The CBC identifies the total number of blood cells
(WBCs, RBCs, and platelets) as well as the hemoglobin, hematocrit (percentage of blood consisting of RBCs), and RBC
indices. Because cellular morphology (shape and
appearance of the cells) is particularly important in most hematologic
disorders, the physician needs to examine the blood cells involved. This
process is referred to as the manual examination of the peripheral smear, which
may be part of the CBC. In this test, a drop of blood is spread on a glass
slide, stained, and examined under a microscope. The shape and size of the RBCs
and platelets as well as the actual appearance of the WBCs provides useful
information in identifying hematologic conditions. Blood for the CBC is
typically obtained by venipuncture.
BONE MARROW ASPIRATION AND BIOPSY
The
bone marrow aspiration and biopsy are crucial when addi-tional information is
needed to assess how an individual’s blood cells are being formed and to assess
the quantity and quality of each type of cell produced within the marrow. These
tests are also used to document infection or tumor within the marrow.
Normal
bone marrow is in a semifluid state and can be aspi-rated through a special
large needle. In adults, bone marrow is usually aspirated from the iliac crest
and occasionally from the sternum. The aspirate provides only a sample of
cells. Aspirate alone may be adequate for evaluating certain conditions, such
as anemia. However, when more information is required, a biopsy is also
performed. Biopsy samples are taken from the posterior iliac crest;
occasionally, an anterior approach is required. A mar-row biopsy shows the
architecture of the bone marrow as well as its degree of cellularity.
Most
patients need no more preparation than a careful expla-nation of the procedure,
but for some very anxious patients, an antianxiety agent may be useful. It is
always important for the physician or nurse to describe and explain to the
patient the pro-cedure and the sensations that will be experienced. The risks,
benefits, and alternatives are also discussed. A signed informed consent is
needed before the procedure is performed.
Before
aspiration, the skin is cleansed as for any minor surgery, using aseptic technique.
Then a small area is anesthetized with a local anesthetic through the skin and
subcutaneous tissue to the periosteum of the bone. It is not possible to
anesthetize the bone itself. The bone marrow needle is introduced with a stylet
in place. When the needle is felt to go through the outer cortex of bone and
enter the marrow cavity, the stylet is removed, a syringe is at-tached, and a
small volume (0.5 mL) of blood and marrow is as-pirated. Patients typically
feel a pressure sensation as the needle is advanced into position. The actual
aspiration always causes sharp but brief pain, resulting from the suction
exerted as the marrow is aspirated into the syringe; the patient should be
forewarned about this. Taking deep breaths or using relaxation techniques often
helps ease the discomfort.
If a
bone marrow biopsy is necessary, it is best performed after the aspiration and
in a slightly different location, because the mar-row structure may be altered
after aspiration. A special biopsy nee-dle is used. Because these needles are
large, the skin is punctured first with a surgical blade to make a 3- or 4-mm
incision. The biopsy needle is advanced well into the marrow cavity. When the
needle is properly positioned, a portion of marrow is cored out, using a twisting
or gentle rocking motion to free the sample and permit its removal within the
biopsy needle. Patients feel a pres-sure sensation but should not feel actual
pain. The nurse should instruct the patient to inform the physician if pain
occurs so that additional anesthetic can be administered.
The major hazard of either bone marrow aspiration or biopsy is a slight risk of bleeding and infection. The bleeding risk is some-what increased if the patient’s platelet count is low or if the patient has been taking a medication (eg, aspirin) that alters platelet function.
After the marrow sample is obtained, pressure is applied to the site for
several minutes. The site is then covered with a sterile dressing. Most
patients have no discomfort after a bone marrow aspiration, but the site of a
biopsy may ache for 1 or 2 days. Warm tub baths and use of a mild analgesic
(eg, acetaminophen) may be useful. Aspirin-containing analgesics should be avoided
because they can aggravate or potentiate any bleeding that may occur.
Related Topics