Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Acquired Thrombophilia - Coagulation Disorders
ACQUIRED
THROMBOPHILIA
Antibodies
to phospholipids are common, acquired causes for thrombophilia (hypercoagulable
states). The most common anti-bodies present against phospholipids are either
lupus or anti-cardiolipin antibodies. Both of these antibodies can be
transient, resulting from infection or certain medications. Most thrombotic
events are venous, but arterial thrombosis can occur in up to one third of the
cases. Patients who persistently test positive for either antibody and who have
had a thrombotic event are at significant risk for recurrent thrombosis
(greater than 50%). Recurrent throm-boses tend to be of the same type—that is,
venous thrombosis after an initial venous thrombosis, arterial thrombosis after
an initial arterial thrombosis.
Another
common acquired cause for thrombophilia is cancer. Specific types of stomach,
pancreatic, lung, and ovarian cancers are most commonly associated with
thrombophilia. The type of thrombosis that results is unusual. Rather than deep
vein throm-bosis or pulmonary embolism, the thrombosis occurs in unusual sites,
such as the portal, hepatic, or renal vein or the inferior vena cava. Migratory
superficial thrombophlebitis or nonbacterial thrombotic endocarditis can also
occur. In these patients, anti-coagulation can be difficult to manage in that
the thrombosis can progress despite standard amounts of anticoagulation.
Medical Management
The
primary method of treating thrombotic disorders is antico-agulation. However,
in thrombophilic conditions, when to treat (prophylaxis or not) and how long to
treat (lifelong or not) can be controversial. Anticoagulation therapy is not
without risks; the most significant risk is bleeding. The most common
anticoagulant medications are identified in the following section.
PHARMACOLOGIC THERAPY
Along
with administering anticoagulant therapy, concerns in-clude minimizing any risk
factors that predispose a patient to thrombosis. When risk factors (eg,
immobility after surgery, pregnancy) cannot be avoided, prophylactic
anticoagulation may be necessary.
Unfractionated Heparin Therapy.
Heparin is a
naturally occurringanticoagulant that enhances AT III and inhibits platelet
function. To prevent thrombosis, heparin is typically given as a subcuta-neous
injection, two or three times daily. To treat thrombosis, heparin is usually
administered intravenously. The therapeutic effect of heparin is monitored by
serial measurements of the acti-vated partial prothrombin time; the dose is
adjusted to maintain the range at 1.5 to 2.5 times the laboratory control. Oral
forms are being evaluated, but their absorption remains variable (Money &
York, 2001).
A
significant potential complication of heparin-based ther-apy is heparin-induced
thrombocytopenia (HIT). Antibodies are formed within the body against the
heparin complex. The actual incidence of HIT is unknown, but it is thought to
occur in as many as 5% patients receiving heparin (Kelton, 1999). Whereas most
patients remain asymptomatic, a significant pro-portion of those individuals
with serologic HIT develop actual thrombocytopenia. A decline in platelet count
typically devel-ops after 5 to 8 days of heparin therapy, and the platelets can
drop significantly, although in most instances the level stays higher than
50,000/mm3. These patients are at
increased risk for thrombosis, either venous or arterial, and the thrombosis
can range from DVT to myocardial infarction, CVA (brain at-tack, stroke), and
ischemic damage to an extremity necessitating amputation. The risk for
development of HIT appears to be increased when heparin is used at higher
concentrations (ie, ther-apeutic versus prophylactic dosage) and with
preexisting comor-bidity, such as underlying cardiac disease.
Low-Molecular-Weight Heparin Therapy.
Low
molecular-weightheparin (LMWH; eg, Dalteparin, Enoxaparin) is a special form of
heparin that has a more selective effect on coagulation. Based on its
biochemical properties, LMWH has a longer half-life and a less variable
anticoagulant response than does standard heparin. These differences permit
LMWH to be safely administered only once or twice daily, without the need for
laboratory monitoring for dose adjustments. The incidence of HIT is much lower
when LMWH is used. In certain conditions, the use of LMWH has allowed
anti-coagulation therapy to be moved entirely to the outpatient setting. Many
cases of uncomplicated DVT are being managed outside the hospital setting. LMWH
is also being increasingly used as “bridge therapy” when patients receiving
anticoagulation therapy (war-farin) require an invasive procedure (eg, biopsy,
surgery). In this sit-uation, warfarin is stopped and LMWH is used in its place
until the procedure is completed. After the procedure, warfarin therapy is
resumed. LMWH is discontinued after a therapeutic level of war-farin is
achieved.
Warfarin (Coumadin) Therapy.
Coumarin
anticoagulants (war-farin; eg, Coumadin) are antagonists of vitamin K and therefore
interfere with the synthesis of vitamin K–dependent clotting factors. Coumarin
anticoagulants bind to albumin, are metabo-lized in the liver, and have an
extremely long half-life. Typically, a patient is initially treated with both
heparin (either the unfrac-tionated form or LMWH) and warfarin. When the
international normalized ratio (INR) reaches the desired therapeutic range, the
heparin is stopped. The dosage required to maintain the therapeutic range (typically
using an INR of 2.0 to 3.0) varies widely among patients and even within the
same patient. Frequent mon-itoring of the INR is extremely important so that
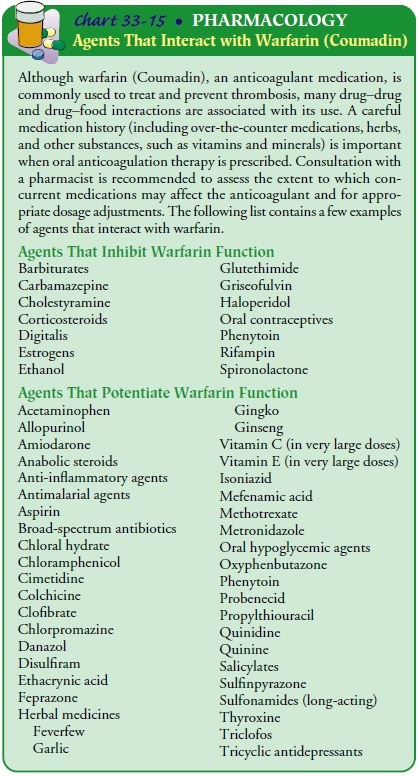
the dosage of warfarin can be adjusted as needed. Warfarin is affected by many
medications; consultation with a pharmacist is important to as-sess the extent
to which concurrently administered medications, herbs, and nutritional
supplements may interact with warfarin. It is also affected by many foods, so
patients need dietary instruc-tion and may benefit from consultation with a
dietitian when re-ceiving warfarin therapy. See Chart 33-15 for a listing of
agents that interact with warfarin.
Nursing Management
Patients with thrombotic disorders should avoid activities that promote circulatory stasis (eg, immobility, crossing the legs). Ex-ercise, especially ambulation, should be performed frequently throughout the day, particularly during long trips by car or plane.
Medications
that alter platelet aggregation, such as low-strength aspirin, may be prescribed.
Some patients require life-long ther-apy with anticoagulants such as warfarin
(eg, Coumadin).
Patients
with thrombotic disorders, particularly those with thrombophilia, should be
assessed for concurrent risk factors for thrombosis and should avoid concomitant
risk factors if possible. For example, use of tobacco and nicotine products
exacerbates the problem and should be avoided.
Just
as for other conditions, patients with thrombotic disor-ders, particularly
thrombophilia, should know the name of their specific condition and understand
its significance. In many in-stances, younger patients with thrombophilia may
not require prophylactic anticoagulation; however, with concomitant risk
fac-tors (eg, pregnancy), increasing age, or subsequent thrombotic events,
prophylactic or lifelong anticoagulation therapy may be re-quired. Being able
to provide the health care provider with an ac-curate health history can be
extremely useful and can help guide the selection of appropriate therapeutic
interventions. Patients with hereditary disorders should be encouraged to have
their sib-lings and children tested for the disorder.
When
patients with thrombotic disorders are hospitalized, fre-quent assessments
should be performed for signs and symptoms of beginning thrombus formation,
particularly in the legs (DVT) and lungs (pulmonary embolism). Ambulation or
range-of-motion ex-ercises as well as the use of elastic compression stockings
should be initiated promptly to decrease stasis. Prophylactic anticoagulants
are commonly prescribed.
Related Topics