Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Idiopathic Thrombocytopenic Purpura (ITP)
IDIOPATHIC
THROMBOCYTOPENIC PURPURA (ITP)
ITP is
a disease that affects people of all ages, but it is more com-mon among
children and young women. There are two forms of ITP: acute and chronic. The
acute form, which occurs predomi-nately in children, often appears 1 to 6 weeks
after a viral illness. This form is self-limited; remission often occurs
spontaneously within 6 months. Occasionally, corticosteroids are needed for a
brief time. Chronic ITP is often diagnosed by exclusion of other causes of
thrombocytopenia.
Pathophysiology
Although
the precise cause remains unknown, viral infections sometimes precede ITP in
children. Occasionally medications such as sulfa drugs can induce ITP. Other
conditions, such as systemic lupus erythematosus (SLE) or pregnancy, can also
induce ITP. Anti-platelet autoantibodies that bind to the patient’s platelets
are found in the blood of patients with ITP. When the platelets are bound by
the antibodies, the RES or tissue macrophage system ingests the platelets,
destroying them. The body attempts to com-pensate for this destruction by increasing
platelet production within the marrow.
Clinical Manifestations
Many
patients have no symptoms, and the low platelet count (often less than
20,000/mm3, and less than 5000/mm3 is not un-common) is an
incidental finding. Common physical manifes-tations are easy bruising, heavy
menses, and petechiae on the extremities or trunk. Patients with simple
bruising or petechiae (“dry purpura”) tend to have fewer complications from
bleeding than those with bleeding from mucosal surfaces, such as the gastrointestinal
tract (including the mouth) and pulmonary sys-tem (eg, hemoptysis), which is
termed “wet purpura.” Patients with wet purpura have a greater risk for
intracranial bleeding than do those with dry purpura. Despite low platelet
counts, the platelets are young and very functional. They adhere to
en-dothelial surfaces and to one another, so spontaneous bleeding does not
always occur.
Assessment and Diagnostic Findings
Patients
may have an isolated decrease in platelets (less than 20,000/mm3 is common), but they
may also have an increase in megakaryocytes (platelet precursors) within the
marrow, as de-tected on bone marrow aspirate.
Medical Management
The
primary goal of treatment is a safe platelet count. Because the risk of
bleeding typically does not increase until the platelet count is lower than
10,000/mm3, patients whose counts
exceed 30,000 to 50,000/mm3 may be carefully observed without additional
intervention. However, if the count is lower than 20,000/mm3, or if bleeding occurs,
the goal is to improve the pa-tient’s platelet count, rather than to cure the
disease. Treatment for ITP usually requires several approaches. If the patient
is tak-ing a medication that is known to cause ITP (eg, quinine,
sulfa-containing medications), that medication must be stopped immediately. The
mainstay of short-term therapy is the use of immunosuppressive agents. The
immunosuppressants block the binding receptors on macrophages so that the
platelets are not destroyed. Prednisone is the agent typically used (at a dose
of 1 mg/kg), and it is effective in about 75% of patients. Cyclophos-phamide
(eg, Cytoxan) and azathioprine (Imuran) can also be used, and dexamethasone
(eg, Decadron) may be effective. Platelet counts rise within a few days after
institution of corti-costeroid therapy; this effect takes longer with
azathioprine. Be-cause of the associated side effects, patients cannot take
high doses of corticosteroids indefinitely. It is not unusual for the platelet
count to drop once the corticosteroid dose is tapered. Some patients can be
successfully maintained on low doses of prednisone (eg, 2.5 to 10 mg every
other day).
Intravenous
gamma globulin (IVIG) is also commonly used to treat ITP. It is effective in
binding the receptors on the macrophages; however, high doses (1 g/kg for 2
days) are re-quired, and the drug is very expensive. Splenectomy is an
alter-native treatment but results in a normal platelet count only 50% of the
time; however, many patients can maintain a “safe” platelet count of more than
30,000/mm3 after removal of the
spleen. Even those who do respond to splenectomy may have recurrences of severe
thrombocytopenia months or years later. Patients who have splenectomy are
permanently at risk for sepsis; these patients should receive Pneumovax, Haemophilus influenzae B, and
meningococcal vaccines, preferably 2 to 3 weeks before the splenectomy is
preferred. Pneumovax vaccine should be repeated at 5- to 10-year intervals.
Other
options for management include use of the chemother-apy agent vincristine (Oncovin).
Vincristine appears to work by blocking the receptors on the macrophages and
therefore in-hibiting platelet destruction; it may also stimulate
throm-bopoiesis. Some data support the efficacy of certain monoclonal
antibodies (eg, rituximab) in increasing platelet counts, but more research is
needed (Stasi, Pagano, Stipa, & Amadori, 2001; Saleh et al., 2000).
Another
approach to the management of chronic ITP involves the use of anti-D (eg,
WinRho) in patients who are Rh(D)-posi-tive. The actual mechanism of action is
unknown. One theory is that the anti-D binds to the patient’s RBCs, which are
in turn de-stroyed by the body’s macrophages. While the macrophages de-stroy
the anti-D/RBC complex, they are not able to destroy platelets. Anti-D produces
a transient decreased hematocrit and increased platelet count in many, but not
all, patients with ITP. Anti-D appears to be most effective in children with
ITP and least effective in patients who have undergone splenectomy.
Despite
the extremely low platelet count, platelet transfusions are usually avoided.
Transfusions tend to be ineffective because the patient’s anti-platelet
antibodies bind with the transfused platelets, causing them to be destroyed.
Platelet counts can actually drop after platelet transfusion. Occasionally,
transfusion of platelets may protect against catastrophic bleeding in patients
with severe wet purpura. Epsilon-aminocaproic acid (EACA; Amicar) may be
use-ful for patients with significant mucosal bleeding refractory to other
treatments.
Nursing Management
Nursing
care for these patients should include an assessment of the patient’s life
style to determine the risk of bleeding from activity. A careful medication
history should also be obtained, including use of over-the-counter medications,
herbs, and nutritional supple-ments. The nurse must be alert for
sulfa-containing medications and medications that alter platelet function (eg,
medications that contain aspirin or other NSAIDs). The nurse should assess for
any history of recent viral illness and reports of headache or visual
dis-turbances (which could be initial symptoms of intracranial bleed-ing).
Patients who are admitted to the hospital with wet purpura and low platelet
counts should have a neurologic assessment in-corporated into their routine
vital sign measurements. No intra-muscular injections or rectal medications
should be administered, and rectal temperature measurements should not be
performed, because they can stimulate bleeding.
Patient
teaching should address signs of exacerbation of disease (petechiae,
ecchymoses); how to contact appropriate health care personnel; the name and
type of medication inducing ITP (if appropriate); current medical treatment
(medications, tapering schedule if relevant, side effects); and the frequency
of monitoring the platelet count. Patients should be instructed to avoid all
agents that interfere with platelet function. The patient should avoid
con-stipation, the Valsalva maneuver (eg, straining at stool), and floss-ing of
the teeth. Electric razors should be used for shaving, and soft-bristled
toothbrushes should replace stiff-bristled ones. Pa-tients should also be
counseled to refrain from vigorous sexual intercourse when the platelet count
is less than 10,000/mm3. Pa-tients who are receiving chronic
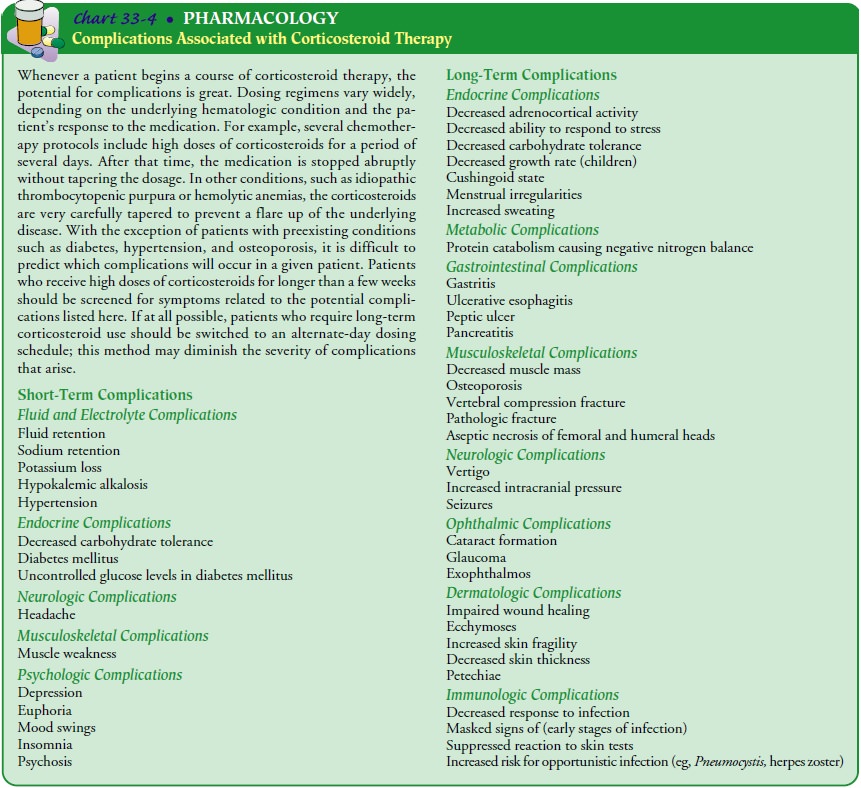
corticosteroids are at risk for complications including osteoporosis, proximal
muscle wasting, cataract formation, and dental caries (see Chart 33-4). Bone
min-eral density should be monitored, and these patients may benefit from
calcium and vitamin D supplementation and bisphosphonate therapy to prevent
significant bone disease.
Related Topics