Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Nursing Process: The Patient With Acute Leukemia
NURSING
PROCESS: THE PATIENT WITH ACUTE LEUKEMIA
Assessment
Although
the clinical picture varies with the type of leukemia in-volved as well as the
treatment implemented, the health history may reveal a range of subtle symptoms
reported by the patient be-fore the problem is manifested by findings on
physical examina-tion. Weakness and fatigue are common manifestations, not only
of the leukemia but also of the resulting complications of anemia and
infection. If the patient is hospitalized, the assessments should be performed
daily, or more frequently as warranted. Because the physical findings may be
subtle initially, a thorough, systematic as-sessment incorporating all body
systems is essential. For example, a dry cough, mild dyspnea, and diminished
breath sounds may in-dicate a pulmonary infection. However, the infection may
not be seen initially on the chest x-ray. The lack of neutrophils delays the
inflammatory response against the pulmonary infection, and it is the
inflammatory response that causes the x-ray changes. The platelet count can
become dangerously low, leaving the patient at risk for significant bleeding.
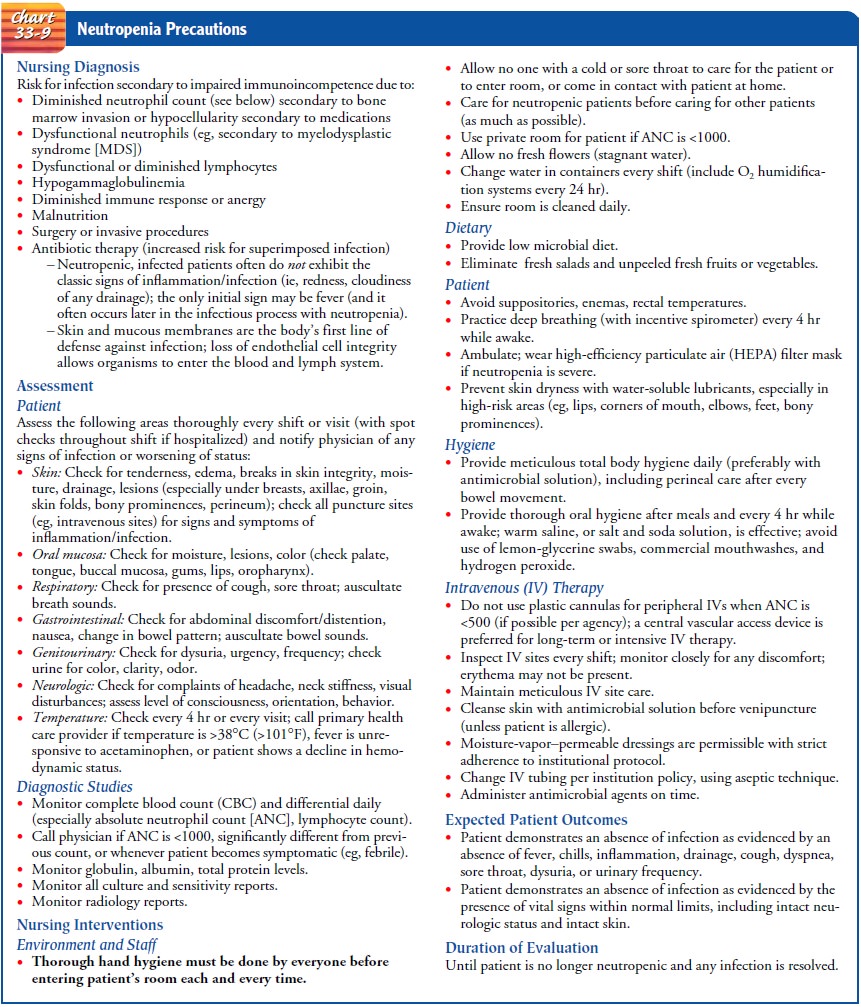
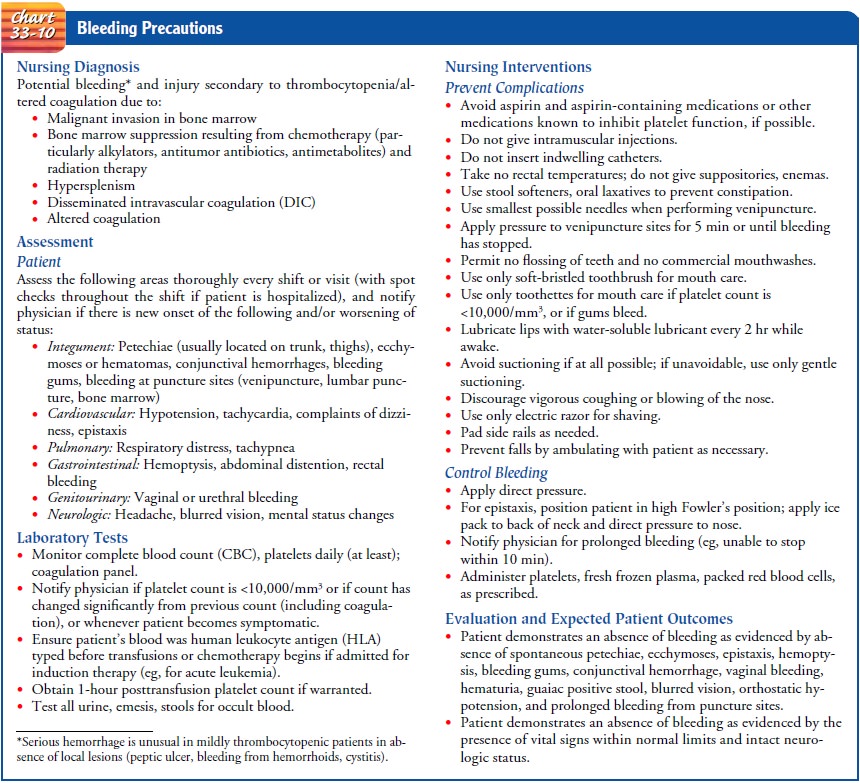
The specific body system assessments are delineated in the neutropenic
precautions and bleeding pre-cautions, found in Charts 33-9 and 33-10,
respectively. When se-rial assessments are performed, current findings are
compared with previous findings to evaluate improvement or worsening.
The nurse also must closely monitor the results of laboratory studies. Flow sheets and spreadsheets are particularly useful in tracking the WBC count, ANC, hematocrit, platelet, and creatinine levels, hepatic function tests, and electrolyte levels. Culture results need to be reported immediately so that appropriate antimicrobial therapy can begin or be modified.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, major nursing diagnoses for the pa-tient with acute
leukemic may include:
•
Risk for infection and bleeding
•
Risk for impaired skin integrity related to toxic
effects of chemotherapy, alteration in nutrition, and impaired mobility
•
Impaired gas exchange
•
Impaired mucous membranes due to changes in
epithelial lining of the gastrointestinal tract from chemotherapy or prolonged
use of antimicrobial medications
•
Imbalanced nutrition, less than body requirements,
related to hypermetabolic state, anorexia, mucositis, pain, and nausea
•
Acute pain and discomfort related to mucositis, WBC
in-filtration of systemic tissues, fever, and infection
•
Hyperthermia related to tumor lysis and infection
•
Fatigue and activity intolerance related to anemia
and infection
•
Impaired physical mobility due to anemia and protective
isolation
•
Risk for excess fluid volume related to renal
dysfunction, hypoproteinemia, need for multiple intravenous medica-tions and
blood products
•
Diarrhea due to altered gastrointestinal flora,
mucosal denudation
•
Risk for deficient fluid volume related to
potential for diar-rhea, bleeding, infection, and increased metabolic rate
•
Self-care deficit due to fatigue, malaise, and
protective isolation
•
Anxiety due to knowledge deficit and uncertain
future
•
Disturbed body image related to change in
appearance, function, and roles
•
Grieving related to anticipatory loss and altered
role func-tioning
•
Potential for spiritual distress
•
Deficient knowledge about disease process,
treatment, com-plication management, and self-care measures
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications that may develop include:
•
Infection
•
Bleeding
•
Renal dysfunction
•
Tumor lysis syndrome
•
Nutritional depletion
•
Mucositis
Planning and Goals
The
major goals for the patient may include absence of com-plications and pain,
attainment and maintenance of adequate nutrition, activity tolerance, ability
for self-care and to cope with the diagnosis and prognosis, positive body
image, and an understanding of the disease process and its treatment.
Nursing Interventions
PREVENTING OR MANAGING INFECTION AND BLEEDING
The
nursing interventions related to diminishing the risk for in-fection and for
bleeding are delineated in Charts 33-9 and 33-10.
MANAGING MUCOSITIS
Although
emphasis is placed on the oral mucosa, it is important to realize that the
entire gastrointestinal mucosa can be altered, not only by the effects of
chemotherapy but also from prolonged ad-ministration of antibiotics. Assessment
of the oral mucosa must be thorough; therefore, dentures must be removed. Areas
to assess in-clude the palate, buccal mucosa, tongue, gums, lips, oropharynx,
and the area under the tongue. In addition to identifying and describing
lesions, the color and moisture of the mucosa should be noted.
Oral
hygiene is very important to diminish the bacteria within the mouth, maintain
moisture, and provide comfort. Soft-bristled toothbrushes should be used until
the neutrophil and platelet counts become very low; at that time, sponge-tipped
applicators should be substituted. Lemon-glycerin swabs and commercial
mouthwashes should never be used because the glycerin and alco-hol within them
are extremely drying to the tissues. Simple rinses with saline (or saline and
baking soda) solutions are inexpensive but effective in cleaning and moistening
the oral mucosa. Because the risk of yeast or fungal infection in the mouth is
great, other medications are often prescribed, such as chlorhexidine rinses
(eg, Peridex) or clotrimazole troches (eg, Mycelex). The nurse re-minds the
patient about the importance of these medications to enhance adherence to the
therapeutic regimen. Chlorhexidine rinses may discolor the teeth.
To
diminish perineal–rectal complications, it is important to cleanse the
perineal–rectal area thoroughly after each bowel movement. Women are instructed
to cleanse the perineum from front to back. Sitz baths are a comfortable method
of cleansing; the perineal–anal region and buttocks must be carefully dried
after-ward to minimize the chance of excoriation. Stool softeners should be
used to increase the moisture of bowel movements; however, the stool texture
must be monitored so that the softeners can be decreased or stopped if the
stool becomes too loose.
IMPROVING NUTRITIONAL INTAKE
The
disease process can increase, and sepsis further increases, the patient’s
metabolic rate and nutritional requirements. Nutri-tional intake is often
reduced because of pain and discomfort as-sociated with stomatitis. Mouth care
before and after meals and administration of analgesics before eating can help
increase in-take. If oral anesthetics are used, the patient must be warned to
chew with extreme care to avoid inadvertently biting the tongue or buccal
mucosa.
Nausea
should not be a major contributing factor, because re-cent advances in
antiemetic therapy are highly effective. However, nausea can result from
antimicrobial therapy, so some antiemetic therapy may still be required after
the chemotherapy has been completed.
Small,
frequent feedings of foods that are soft in texture and moderate in temperature
may be better tolerated. Low-microbial diets are typically prescribed (avoiding
uncooked fruits or vegetables and those without a peelable skin). Nutritional
sup-plements are frequently used. Daily body weights (as well as in take and
output measurements) are useful in monitoring fluid status.
Calorie
counts are useful, as are more formal nutritional assess-ments. Parenteral
nutrition is often required to maintain adequate nutrition.
EASING PAIN AND DISCOMFORT
Recurrent
fevers are common in acute leukemia; at times, they are accompanied by shaking
chills, which can be severe (rigors). Myalgias and arthralgias can result.
Acetaminophen is typically given to decrease fever, but it does so by
increasing diaphoresis. Sponging with cool water may be useful, but cold water
or ice packs should be avoided because the heat cannot dissipate from
constricted blood vessels. Bedclothes need frequent changing as well. Gentle
back and shoulder massage may provide comfort.
Stomatitis
can also cause significant discomfort. In addition to oral hygiene practices,
patient-controlled analgesia can be effective in controlling the pain.
Because
patients with acute leukemia require hospitalization for extensive nursing care
(either during induction or consolida-tion therapy or during resultant
complications), sleep deprivation frequently results. Nurses need to implement
creative strategies that permit uninterrupted sleep for at least a few hours
while still administering necessary medications on time.
With
the exception of severe mucositis, less pain is associated with acute leukemia
than with many other forms of cancer. How-ever, the amount of psychologic
suffering that the patient must en-dure can be immense. Patients greatly benefit
from active listening.
DECREASING FATIGUE AND DECONDITIONING
Fatigue
is a common and oppressive problem. Nursing interven-tions should focus on
assisting the patient to establish a balance be-tween activity and rest.
Patients with acute leukemia need to maintain some physical activity and
exercise to prevent the decon-ditioning that results from inactivity. Use of a
high-efficiency par-ticulate air (HEPA) filter mask can permit the patient to
ambulate outside the room despite severe neutropenia. Although many pa-tients
lack the motivation to use them, stationary bicycles within the room can also
be used. At a minimum, patients should be en-couraged to sit up in a chair
while awake rather than staying in bed; even this simple activity can improve the
patient’s tidal volume and enhance circulation. Physical therapy can also be
beneficial.
MAINTAINING FLUID AND ELECTROLYTE BALANCE
Febrile
episodes, bleeding, and inadequate or overly aggressive fluid replacement can
alter the patient’s fluid status. Similarly, persistent diarrhea, vomiting, and
long-term use of certain anti-microbial agents can cause significant deficits
in electrolytes. In-take and output need to be measured accurately, and daily
weights should also be monitored. The patient should be assessed for signs of
dehydration as well as fluid overload, with particular at-tention to pulmonary
status and the development of dependent edema. Laboratory test results,
particularly electrolytes, blood urea nitrogen, creatinine, and hematocrit,
should be monitored and compared with previous results. Replacement of
electrolytes, par-ticularly potassium and magnesium, is commonly required.
Pa-tients receiving amphotericin or certain antibiotics are at increased risk
for electrolyte depletion.
IMPROVING SELF-CARE
Because
hygiene measures are so important in this patient popu-lation, they must be
performed by the nurse when the patient can-not do so. However, the patient
should be encouraged to do as much as possible, to preserve mobility and
function as well as self-esteem. Patients may have negative feelings, even
disgust that they can no longer care for themselves. Empathetic listening is
helpful, as is realistic reassurance that these deficits are temporary. As the
patient recovers, it is important to assist him or her to resume more
self-care. Patients are usually discharged from the hospital with a central
vascular access device (eg, Hickman catheter, PICC), and most patients can care
for the catheter with adequate instruction and practice under observation.
MANAGING ANXIETY AND GRIEF
Being
diagnosed with acute leukemia can be extremely frighten-ing. In many instances,
the need to begin treatment is emergent, and patients have little time to
process the fact that they have the illness before making decisions about
therapy. Providing emo-tional support and discussing the uncertain future are
crucial. The nurse also needs to assess how much information patients want to
have regarding the illness, its treatment, and potential complications. This
desire should be reassessed at intervals, be-cause needs and interest in
information change throughout the course of the disease and treatment.
Priorities must be identified so that procedures, assessments, and self-care
expectations are adequately explained even to those who do not wish extensive
information.
Many
patients become depressed and begin to grieve for the losses they feel, such as
normal family functioning, professional roles and responsibilities, and social
roles, as well as physical func-tioning. Nurses can assist patients to identify
the source of the grief and encourage them to allow time to adjust to the major
life changes produced by the illness. Role restructuring, in both fam-ily and
professional life, may be required. Again, when possible, permitting patients
to identify options and to take time making significant decisions regarding
such restructuring is helpful.
Discharge
from the hospital can also provoke anxiety. Although most patients are
extremely eager to go home, they may lack con-fidence in their ability to
manage potential complications and to resume their normal activity. Close
communication between nurses across care settings can reassure patients that
they will not be abandoned.
ENCOURAGING SPIRITUAL WELL-BEING
Because
acute leukemia is a serious, potentially life-threatening illness, the nurse
may offer support to enhance the patient’s spir-itual well-being. The patient’s
spiritual and religious practices should be assessed and pastoral services
offered. Throughout the patient’s illness, it is important that the nurse
assist the patient to maintain hope. However, that hope should be realistic and
will certainly change over the course of the illness. For example, the patient
may initially hope to be cured, but with repeated relapses and a change to
terminal care the same patient may hope for a quiet, dignified death.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Nursing
interventions for potential complications were described previously.
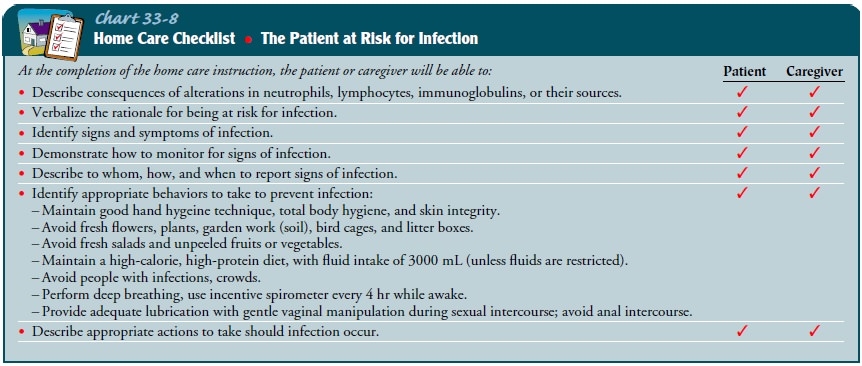
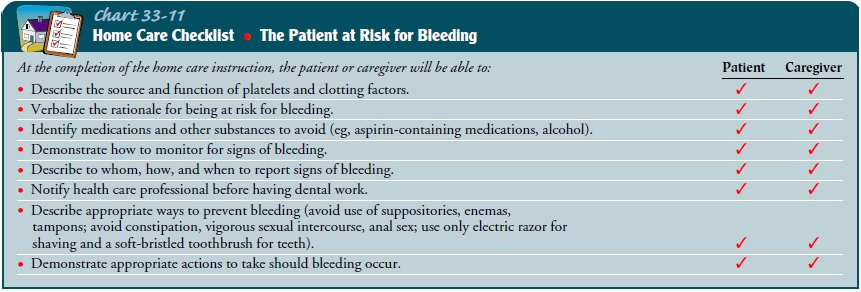
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Most
patients cope better when they have an understanding of what is happening to
them. Based on their education, literacy level, and interest, teaching of
patient and family should focus on the disease (including some pathophysiology),
its treatment, and certainly the significant risk for infection and bleeding
(Charts 33-8 and 33-11) that results.
Management
of a vascular access device can be taught to most patients or family members.
Follow-up and care for the devices may also need to be provided by nurses in an
outpatient facility or by a home care agency or a health care providerv.
Continuing Care.
Shortened
hospital stays and outpatient carehave significantly altered care for patients
with acute leukemia. In many instances, when the patient is clinically stable
but still re-quires parenteral antibiotics or blood products, these procedures
can be performed in an outpatient setting. Nurses in these vari-ous settings
must communicate regularly. Patients need to learn which parameters are
important for them to monitor, and how to monitor them. Specific instructions
need to be given as to when the patient should seek care from the physician or
a health care provider.
Patients
and their families need to have a clear understand-ing of the disease and the
prognosis. The nurse acts as an advo-cate to ensure that this information is
provided. When patients no longer respond to therapy, it is important to
respect their choices about treatment, including measures to prolong life and
other end-of-life measures. Advance directives and living wills provide
patients with some measure of control during terminal illness.
Many
patients in this stage still choose to be cared for at home, and families often
need support when considering this option. Coordination of home care services
and instruction can help to alleviate anxiety about managing the patient’s care
in the home. As the patient becomes weaker, the caregivers must assume more of
the patient’s care. In addition, caregivers often need to be en-couraged to
take care of themselves, allowing time for rest and ac-cepting emotional
support. Hospice staff can assist in providing respite for family members as
well as care for the patient. Patients and families also need assistance to
cope with changes in their roles and responsibilities. Anticipatory grieving is
an essential task during this time.
In
patients with acute leukemia, death typically occurs from infection or
bleeding. Family members need to have informa-tion about these complications
and the measures to take should either occur. Many family members cannot cope
with the care required when a patient begins to bleed actively. It is important
to delineate alternatives to keeping the patient at home. Should another option
be sought, family members who may feel guilty that they could not keep the
patient at home will require sup-port from the nurse.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Shows no evidence of
infection
2) Experiences no bleeding
3) Has intact oral mucous
membranes
a) Participates in oral
hygiene regimen
b) Reports no discomfort in
mouth
4) Attains optimal level of
nutrition
a) Maintains weight with
increased food and fluid intake
b) Maintains adequate
protein stores (albumin)
5) Reports satisfaction
with pain and discomfort levels
6) Has less fatigue and
increased activity
7) Maintains fluid and
electrolyte balance
8) Participates in
self-care
9) Copes with anxiety and
grief
a) Discusses concerns and
fears
b) Uses stress management
strategies appropriately
c) Participates in
decisions regarding end-of-life care
10) Absence of complications
Related Topics