Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Iron Deficiency Anemia
Hypoproliferative Anemias
IRON
DEFICIENCY ANEMIA
Iron
deficiency anemia typically results when the intake of dietary iron is
inadequate for hemoglobin synthesis. The body can store about one fourth to one
third of its iron, and it is not until those stores are depleted that iron
deficiency anemia actually begins to develop. Iron deficiency anemia is the
most common type of ane-mia in all age groups, and it is the most common anemia
in the world. More than 500 million people are affected, more com-monly in
underdeveloped countries, where inadequate iron stores can result from
inadequate intake of iron (seen with vegetarian diets) or from blood loss (eg,
from intestinal hookworm). Iron deficiency is also common in the United States.
In children, ado-lescents, and pregnant women, the cause is typically
inadequate iron in the diet to keep up with increased growth. However, for most
adults with iron deficiency anemia, the cause is blood loss. In fact, in
adults, the cause of iron deficiency anemia should be considered to be bleeding
until proven otherwise.
The
most common cause of iron deficiency in men and post-menopausal women is
bleeding (from ulcers, gastritis, inflamma-tory bowel disease, or
gastrointestinal tumors). The most common cause of iron deficiency anemia in
premenopausal women is men-orrhagia (excessive menstrual bleeding) and
pregnancy with in-adequate iron supplementation. Patients with chronic
alcoholism often have chronic blood loss from the gastrointestinal tract, which
causes iron loss and eventual anemia. Other causes include iron malabsorption,
as is seen after gastrectomy or with celiac disease.
Clinical Manifestations
Patients
with iron deficiency primarily have the symptoms of ane-mia. If the deficiency
is severe or prolonged, they may also have a smooth, sore tongue, brittle and
ridged nails, and angular cheilosis (an ulceration of the corner of the mouth).
These signs subside after iron-replacement therapy. The health history may be
significant for multiple pregnancies, gastrointestinal bleeding, and pica (a
craving for unusual substances, such as ice, clay, or laundry starch).
Assessment and Diagnostic Findings
The
most definitive method of establishing the diagnosis of iron deficiency anemia
is bone marrow aspiration. The aspirate is stained to detect iron, which is at
a low level or even absent. However, few patients with suspected iron
deficiency anemia undergo bone marrow aspiration. In many patients, the
diagnosis can be established with other tests, particularly in patients with a
history of conditions that predispose them to this type of anemia.
There
is a strong correlation between laboratory values mea-suring iron stores and
levels of hemoglobin. After the iron stores are depleted (as reflected by low
serum ferritin levels), the hemo-globin level falls. The diminished iron stores
cause small RBCs. Therefore, as the anemia progresses, the MCV, which measures
the size of the RBC, also decreases. Hematocrit and RBC levels are also low in
relation to the hemoglobin level. Other laboratory tests that measure iron
stores are useful but are not as consistent indicators as a low ferritin level,
which reflects low iron stores. Typically, patients with iron deficiency anemia
have a low serum iron level and an elevated TIBC, which measures the transport
protein supplying the marrow with iron as needed (also referred to as
transferrin). However, other disease states, such as infection and inflammatory
conditions, can also cause a low serum iron level and TIBC with an elevated
ferritin level. Therefore, the most reliable laboratory findings in evaluating
iron deficiency anemia are the ferritin and hemoglobin values.
Medical Management
Except
in the case of pregnancy, the cause of iron deficiency should be investigated.
Anemia may be a sign of a curable gastro-intestinal cancer or of uterine
fibroid tumors. Stool specimens should be tested for occult blood. People 50
years of age or older should have a colonoscopy, endoscopy, or other
examination of the gastrointestinal tract to detect ulcerations, gastritis,
polyps, or cancer. Several oral iron preparations—ferrous sulfate, ferrous
gluconate, and ferrous fumarate—are available for treating iron deficiency
anemia. In some cases, oral iron is poorly absorbed or poorly tolerated, or
iron supplementation is needed in large amounts. In these situations, intravenous
or intramuscular admin-istration of iron dextran may be needed. Before
parenteral administration of a full dose, a small test dose should be
adminis-tered to avoid the risk of anaphylaxis with either intravenous or
in-tramuscular injections. Emergency medications (eg, epinephrine) should be
close at hand.If no signs of allergic reaction have occured after 30 minutes,
the remaining dose of iron may be administered. Several doses are required to
replenish the patient’s iron stores.
Nursing Management
Preventive
education is important, because iron deficiency anemia is common in
menstruating and pregnant women. Food sources high in iron include organ meats
(beef or calf’s liver, chicken liver), other meats, beans (black, pinto, and
garbanzo), leafy green veg-etables, raisins, and molasses. Taking iron-rich
foods with a source of vitamin C enhances the absorption of iron.
The
nurse helps the patient select a healthy diet. Nutritional counseling can be
provided for those whose usual diet is inade-quate. Patients with a history of
eating fad diets or strict vegetar-ian diets are counseled that such diets
often contain inadequate amounts of absorbable iron. The nurse encourages
patients to con-tinue iron therapy as long as it is prescribed, although they
may no longer feel fatigued.
Because
iron is best absorbed on an empty stomach, patients should be advised to take
the supplement an hour before meals. Most patients can use the less expensive,
more standard forms of ferrous sulfate. Tablets with enteric coating may be
poorly
absorbed
and should be avoided. Other patients have difficulty taking iron supplements
because of gastrointestinal side effects (primarily constipation, but also
cramping, nausea, and vomiting). Some iron formulations are designed to limit
gastrointestinal side effects by the addition of a stool softener or use of
sustained-release formulations to limit nausea or gastritis. Specific patient
teaching aids, such as the accompanying patient education guide (Chart 33-2),
can assist patients with the use of iron supplements.
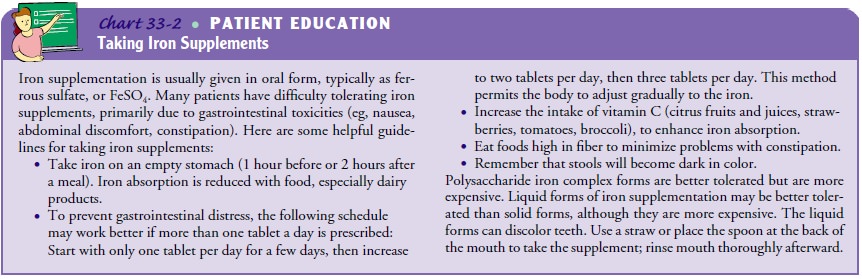
If
taking iron on an empty stomach causes gastric distress, the patient may need
to take the iron supplement with meals. How-ever, doing so diminishes iron
absorption by as much as 50%, thus prolonging the time required to replenish
iron stores. Antacids or dairy products should not be taken with iron, because
they greatly diminish the absorption of iron. Polysaccharide iron complex forms
that have less gastrointestinal toxicity are also available, but they are more
expensive.
Liquid
forms of iron that cause less gastrointestinal distress are available. However,
they can stain the teeth; patients should be in-structed to take this
medication through a straw, to rinse the mouth with water, and to practice good
oral hygiene after taking this med-ication. Finally, patients should be
informed that iron salts may color the stool dark green or black. However, iron
replacement therapy does not cause a false-positive result on stool analyses for
occult blood.
Intramuscular
supplementation is used infrequently. The vol-ume of iron required may be
excessive. The intramuscular injec-tion causes some local pain and can stain
the skin. These side effects are minimized by using the Z-track technique for
administering iron dextran deep into the gluteus maximus muscle (buttock).
Avoid vigorously rubbing the injection site after the injection. Be-cause of
the problems with intramuscular administration, the in-travenous route is
preferred for administration of iron dextran.
Related Topics