Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
HodgkinŌĆÖs Disease
The Lymphomas
The
lymphomas are neoplasms of cells of lymphoid origin. These tumors usually start
in lymph nodes but can involve lymphoid tissue in the spleen, the
gastrointestinal tract (eg, the wall of the stomach), the liver, or the bone
marrow. They are often classified according to the degree of cell
differentiation and the origin of the predominant malignant cell. Lymphomas can
be broadly clas-sified into two categories: HodgkinŌĆÖs disease and non-HodgkinŌĆÖs
lymphoma (NHL).
HODGKINŌĆÖS
DISEASE
HodgkinŌĆÖs
disease is a relatively rare malignancy that has an im-pressive cure rate. It
is somewhat more common in men than women and has two peaks of incidence: one
in the early 20s and the other after 50 years of age. Unlike other lymphomas,
HodgkinŌĆÖs disease is unicentric in origin in that it initiates in a sin-gle
node. The disease spreads by contiguous extension along the lymphatic system.
The cause of HodgkinŌĆÖs disease is unknown, but a viral etiology is suspected.
In fact, fragments of the Epstein-Barr virus have been found in 40% to 50% of
patients; this occurs more commonly in the younger patient population (Weiss,
2000). There is a familial pattern associated with HodgkinŌĆÖs disease:
first-degree relatives have a higher-than-normal frequency of the dis-ease.
There is no increased incidence documented for non-blood relatives (eg,
spouses).
The
malignant cell of HodgkinŌĆÖs disease is the Reed-Sternberg cell, a gigantic
tumor cell that is morphologically unique and is thought to be of immature
lymphoid origin. It is the pathologic hallmark and essential diagnostic
criterion for HodgkinŌĆÖs disease. However, the tumor is very heterogeneous and
may actually con-tain few Reed-Sternberg cells. Repeated biopsies may be
required to establish the diagnosis.
HodgkinŌĆÖs disease is customarily classified
into five subgroups based on pathologic analyses that reflect the natural
history of the malignancy and suggest the prognosis. For example, when
lym-phocytes predominate, with few Reed-Sternberg cells and minimal involvement
of the lymph nodes, the prognosis is much more fa-vorable than when the
lymphocyte count is low and the lymph nodes are virtually replaced by tumor
cells of the most primitive type. The majority of patients with HodgkinŌĆÖs
disease have the types currently designated ŌĆ£nodular sclerosisŌĆØ or ŌĆ£mixed
cellularity.ŌĆØ The nodular sclerosis type tends to occur more often in young
women, at an earlier stage but with a worse prognosis than the mixed
cellu-larity subgroup, which occurs more commonly in men and causes more
constitutional symptoms but has a better prognosis.
Clinical Manifestations
HodgkinŌĆÖs
disease usually begins as a painless enlargement of one or more lymph nodes on
one side of the neck. The individual nodes are painless and firm but not hard.
The most common sites for lymphadenopathy are the cervical, supraclavicular,
and medi-astinal nodes; involvement of the iliac or inguinal nodes or spleen is
much less common. A mediastinal mass may be seen on chest x-ray; occasionally,
the mass is large enough to compress the trachea and cause dyspnea. Pruritus is
common; it can be extremely dis-tressing, and the cause is unknown. Approximately
20% of patients experience brief but severe pain after drinking alcohol
(Cavalli, 1998). The pain is usually at the site of the HodgkinŌĆÖs disease;
again, the cause is unknown.
All
organs are vulnerable to invasion by HodgkinŌĆÖs disease. The symptoms result
from compression of organs by the tumor, such as cough and pulmonary effusion
(from pulmonary infiltrates), jaundice (from hepatic involvement or bile duct
obstruction), ab-dominal pain (from splenomegaly or retroperitoneal
adenopathy), or bone pain (from skeletal involvement). Herpes zoster infections
are common. A cluster of constitutional symptoms has important prognostic
implications. Referred to as ŌĆ£B symptoms,ŌĆØ they include fever (without chills),
drenching sweats (particularly at night), and unintentional weight loss of more
than 10%. ŌĆ£B symptomsŌĆØ are found in 40% of patients and are more common in
advanced disease.
A mild
anemia is the most common hematologic finding. The WBC count may be elevated or
decreased. The platelet count is typically normal, unless the tumor has invaded
the bone marrow, suppressing hematopoiesis. The erythrocyte sedimentation rate(ESR) and the serum copper level are
used by some clinicians toassess disease activity. Patients with HodgkinŌĆÖs
disease have im-paired cellular immunity, as evidenced by an absent or
decreased reaction to skin sensitivity tests (eg, Candida, mumps).
Assessment and Diagnostic Findings
Because
many manifestations are similar to those occurring with infection, diagnostic
studies are performed to rule out an infectious origin for the disease. The
diagnosis is made by means of an exci-sional lymph node biopsy and the finding
of the Reed-Sternberg cell. Once the diagnosis is confirmed and the histologic
type is es-tablished, it is necessary to assess the extent of the disease, a
process referred to as staging.During the health history, the nurse should assess
for any ŌĆ£B symptoms.ŌĆØ Physical examination requires a careful, systematic
evaluation of the lymph node chains, as well as the size of the spleen and
liver. A chest x-ray and a CT scan of the chest, abdomen, and pelvis are
crucial to identify the extent of lymphadenopathy within these regions.
Laboratory tests include CBC, platelet count, ESR, and liver and renal function
studies. A bone marrow biopsy is per-formed if there are signs of marrow
involvement, and some physi-cians routinely perform bilateral biopsies. Bone
scans may be performed to identify any involvement in these areas. A staging
la-parotomy and lymphangiography are no longer considered manda-tory, primarily
because of the accuracy of CT.
Medical Management
The
general intent in treating HodgkinŌĆÖs disease, regardless of stage, is cure.
Treatment is determined primarily by the stage of the disease, not the
histologic type; however, extensive research is ongoing to target treatment
regimens to histologic subtypes or prognostic features. Traditionally, early
HodgkinŌĆÖs disease was treated by a staging laparotomy followed by radiation
therapy. Re-cent data show improved results and decreased complications with a
short course (2 to 4 months) of chemotherapy followed by radi-ation therapy in
certain subsets of early-stage disease (IA and IIA); patients with early-stage
disease and good prognostic features may receive radiation therapy alone (Hoppe
et al., 2000). Combina-tion chemotherapy, for example with doxorubicin
(Adriamycin), bleomycin (Blenoxane), vinblastine (Velban), and dacarbazine
(DTIC), referred to as ABVD, is now the standard treatment for more advanced
disease (stages III and IV and all B stages).
Radiation
therapy is still very useful for patients with exten-sive adenopathy (often
termed bulky disease). In this group, residual disease often persists after the
chemotherapy treatment is finished; radiation therapy to the areas of remaining
adenopathy has been shown to improve survival.
Even
when HodgkinŌĆÖs disease does recur, the use of high doses of chemotherapeutic
agents, followed by autologous BMT or stem cell transplantation (PBSCT), can be
very effective in controlling the disease and extending survival time.
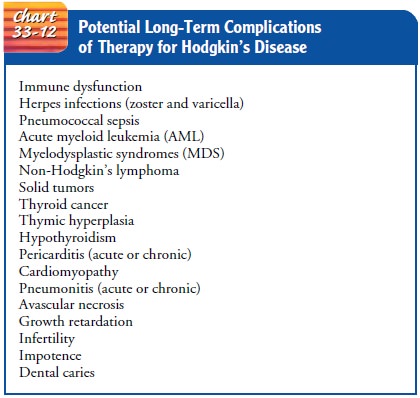
Long-Term Complications of Therapy
Much
is now known about the long-term effects of chemotherapy and radiation therapy,
primarily from the large numbers of peo-ple who were cured of HodgkinŌĆÖs disease
by these treatments. The various complications of treatment are listed in Chart
33-12. Risk factors for other cancers should be assessed, and long-term
sur-veillance is crucial. The potential development of a second malig-nancy is
obviously of concern to patients, and this potential should be addressed with
the patient when treatment decisions are made. However, it is important to
consider that HodgkinŌĆÖs disease is cur-able. Revised treatment approaches are
aimed at diminishing the risk for complications without sacrificing the
potential for cure.
Related Topics