Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hematologic Disorders
Aplastic Anemia
APLASTIC
ANEMIA
Aplastic
anemia is a rather rare disease caused by a decrease in or damage to marrow
stem cells, damage to the microenvironment within the marrow, and replacement
of the marrow with fat. It re-sults in bone marrow aplasia (markedly reduced hematopoiesis). Therefore, in addition to
severe anemia, significant neutropenia and thrombocytopenia (a deficiency of
platelets) are also seen.
Pathophysiology
Aplastic
anemia can be congenital or acquired, but most cases are idiopathic (ie,
without apparent cause). Infections and pregnancy can trigger it, or it may be
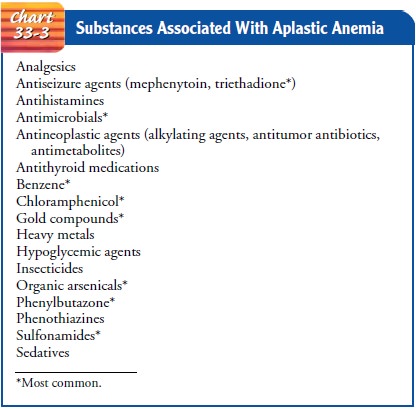
caused by certain medications, chem-icals, or radiation damage (Chart 33-3).
Agents that regularly produce marrow aplasia include benzene and benzene
derivatives (eg, airplane glue). Certain toxic materials, such as inorganic
ar-senic and several pesticides (including DDT, which is no longer used or
available in the United States), have also been implicated as potential causes.
Various medications have been associated with aplastic anemia.
Clinical Manifestations
The manifestations of aplastic anemia are often insidious. Com-plications resulting from bone marrow failure may occur before the diagnosis is established.
Typical complications are infection and symptoms of
anemia (eg, fatigue, pallor, dyspnea). Purpura (bruising) may develop later and
should trigger a CBC and hema-tologic evaluation if these were not performed
initially. If the patient has had repeated throat infections, cervical
lymphaden-opathy may be seen. Other lymphadenopathies and splenomegaly
sometimes occur. Retinal hemorrhages are common.
Assessment and Diagnostic Findings
In
many situations, aplastic anemia occurs when a medication or chemical is
ingested in toxic amounts. However, in a few people, it develops after a
medication has been taken at the recommended dosage. This may be considered an
idiosyncratic reaction in those who are highly susceptible, possibly caused by
a genetic defect in the medication biotransformation or elimination process. A
bone marrow aspirate shows an extremely hypoplastic or even aplastic (very few
to no cells) marrow replaced with fat.
Medical Management
It is
presumed that the lymphocytes of patients with aplastic ane-mia destroy the
stem cells and consequently impair the produc-tion of RBCs, WBCs, and
platelets. Despite its severity, aplastic anemia can be successfully treated in
most people. Potentially, those who are younger than 60 years of age, who are
otherwise healthy, and who have a compatible donor can be cured of the dis-ease
by a bone marrow transplantaton (BMT) or peripheral stem cell transplantation
(BSCT). In others, the disease can be managed with immunosuppressive therapy. A
combination of antithymo-cyte globulin and cyclosporine is used most commonly.
Immuno-suppressants prevent the patient’s lymphocytes from destroying the stem
cells. If relapse occurs (ie, the patient becomes pancy-topenic again), reinstitution
of the same immunologic agents may induce another remission. Corticosteroids
are not very useful as an immunosuppressive agent, because patients with
aplastic anemia appear particularly susceptible to the development of bone
com-plications from corticosteroids (ie, aseptic necrosis of the head of the
femur).
Supportive
therapy plays a major role in the management of aplastic anemia. Any offending
agent is discontinued. The patient is supported with transfusions of RBCs and
platelets as necessary. Death usually is caused by hemorrhage or infection.
Nursing Management
Patients
with aplastic anemia are vulnerable to problems related to RBC, WBC, and
platelet deficiencies. They should be assessed carefully for signs of infection
and bleeding. Specific interven-tions are delineated in the sections on
neutropenia and thrombo-cytopenia.
Related Topics