Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Skeletal System and Joints
The Skeletal System
The Skeletal System
BONE FUNCTIONS
The primary function of bone is to be a supporting framework for the rest of the body. It is often com-pared to the steel girders that support buildings. But, unlike steel girders, bone is one of the most metabol-ically active tissue; remaining active throughout life and having the capacity to change shape and density according to mechanical demands. Bone contributes to the shape and positioning of the various structures of the body. Together, some bones protect important organs. The heart and lungs, for example, lie securely in the bony thoracic cage. The brain lies in the pro-tective cranial cavity made up of many bones.
The bones, with their joints, act as levers that are manipulated by the muscles attached to them and po-sitioned across the joints. Bones are the main reser-voir for minerals, such as calcium and phosphorus. Calcium is an important mineral required for con-duction of impulses in nerves, muscle contraction, and clotting of blood. It is vital for the body to main-tain the blood levels of calcium within a narrow range, and bone serves as a reservoir when the blood levels of calcium fluctuate. Bone is also a factory where blood cells are manufactured, and bone may also be considered as one of the sites where fat is stored because yellow bone marrow is primarily adi-pose tissue.
STRUCTURE AND FORMATION OF BONE
Bone is a special form of connective tissue. Similar to other connective tissue, it has ground substance with collagen fibers and cells . However, the ground substance in bone has a large deposition of calcium and phosphorus that makes the tissue hard and rigid. The minerals are in the form of hydroxya-patite crystals (calcium carbonate and calciumphosphate mineral salts). Minerals account for 60% to 70% of the dry weight of bone; water accounts for 5% to 8%; and organic matter, the remaining weight. The collagen fibers are arranged in various direc-tions, with the arrangement being altered according to lines of stress and tension created by the weight and activity of the body. The presence of collagen fiber gives bone its flexibility and resilience. Collagen fibers and minerals combined make the bone flexible, compressible, and able to withstand considerable shear forces. The gel-like ground substance that sur-rounds the collagen fibers is made up of large, com-plex molecules called proteoglycans.Proteoglycans are mucopolysaccharides bound to protein chains.
Like all tissue, bone requires its own supply of blood and nerves. Unlike other softer tissue, bone is solid and must grow around blood vessels and nerves in a more complex process. To better understand this complex process, bone formation in the fetus must be examined. The process of bone formation is known as ossification, osteogenesis, or calcification (see Figure 3.1). Ossification may occur in two ways. In intramembranous ossification, bone is formedwithin or on fibrous connective tissue membranes. Flat bones of the skull and mandible are formed by intramembranous ossification. In endochondral os-sification, the more common type of ossification,bone is formed within hyaline cartilage.
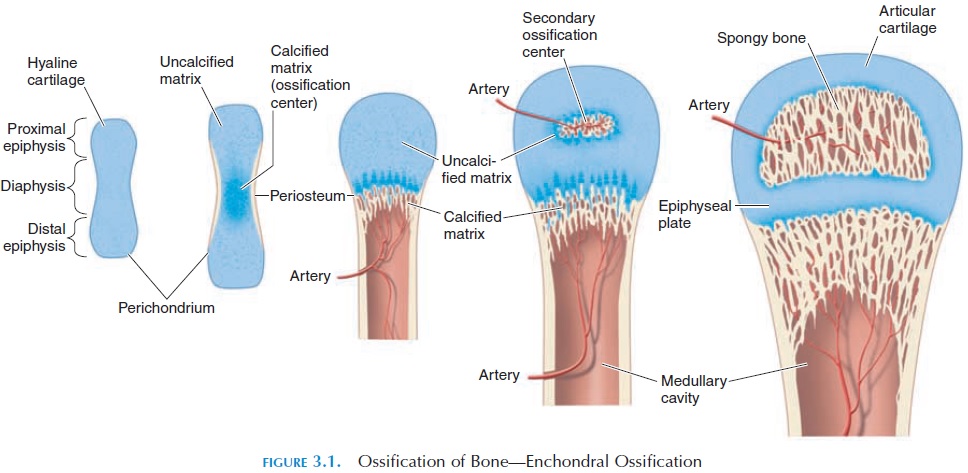
In the fetus, special cells known as chondroblasts appear in areas where bone must be present. Chon-droblast secretions result in the formation of carti-lage, which eventually takes the precise shape of bone in that area. In this way, cartilage forms a mold in which minerals can be deposited to form bone. The connective tissue around the cartilage forms a highly vascular membrane around the mold. Nerves are also incorporated in the membrane. The mem-brane has many chondroblasts, which help cartilagi-nous growth on the surface of the model. This mem-brane is known as the perichondrium.
At a later stage, chondroblasts undergo transfor-mation and begin to secrete the chemicals that pre-cipitate deposition of minerals around them. The transformed cells areosteoblasts.
The chondroblasts in the membrane are also trans-formed and bone begins to form both inside and on the surface of the cartilage model.
The beginning and rate of ossification varies from bone to bone. In each bone, ossification may begin at different sites known as ossification centers. Ossifi-cation continues until the cartilage model has been replaced by bone. The bone has the potential to grow in length as long as adjacent ossification centers have not fused together. Once fused, the bone can only be-come thicker.
A typical bone has a hard outer shell, with a blood and nerve supply known as the periosteum, which is actually ossified perichondrium. Because the blood and nerve supply are located here, the periosteum is an important component of bone. It also houses the osteogenic cells (cells that divide to form os-teoblasts) and osteoblasts that are required for new bone formation on the surface, according to stresses and strains placed on the bone. The fusion of bones that occur in some regions of the body is also a result of the presence of periosteum. In addition, ligaments that cross joints are fused with the periosteum of ad-jacent bones, adding to joint stability. Tendons of muscles also blend with the collagen fibers of the periosteum at the point of attachment.
BONE REMODELING
For bone to grow and rearrange collagen fibers and minerals in lines of stress, two processes—one that builds and another that removes—must be in place. While osteoblasts help with bone formation, another group of cells (osteoclasts) reabsorb bone. In this way, the bone retains its shape and grows without be-coming thicker.
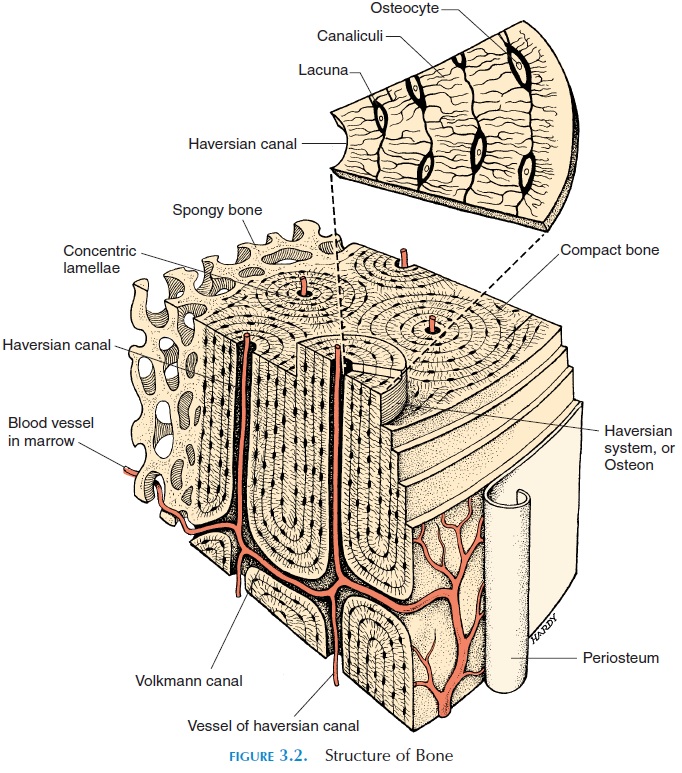
Normally, the outer layer of bone is dense and is known as compact, or cortical, bone. Internally, the bone is less dense, with bone spicules surrounded by spaces filled with red marrow. This is the spongy, can-cellous, or trabecular bone. Spongy bone is found inlarger amounts in short, flat, and irregularly shaped bones. A bone marrow cavity, or medullary cavity,may be found at the center of the bone. Cortical bone always surrounds cancellous bone, but the quantity of each type varies. About 75% of the bones in the body are compact. Because compact bone is solid, blood vessels that supply the cells with nutrients and nerves are contained in canals. The canals that run trans-versely from the periosteum are the perforating, or Volkmann’s, canals. These canals connect with otherthe haversian canals, canals that run longitudinally through the compact bone. The collagen fibers are arranged in lamellae, concentric layers around the canals forming cylinders called osteons or haversiansystems. The osteoblasts surrounded by calcified ma-trix in the compact bone are the osteocytes. They are located in small cavities known as lacunae. The lacu-nae communicate with other adjacent lacunae by tiny canals (canaliculi) that ramify throughout the bone connecting adjacent cells (see Figure 3.2) and the haversian canals. The osteocytes, therefore, obtain nu-trients from the blood vessels in the haversian canals.
PARTS OF A LONG BONE
The activity of osteoclasts and osteoblasts is particu-larly rapid at the ends of long bones that extend in length. The region (see Figure 3.3) at the ends of bones is theepiphysis (plural, epiphyses). New carti-lage is constantly being formed here to increase the length. Adjacent to this new cartilage, is a thin region known as theepiphyseal plate, where the os-teoblasts constantly turn cartilage into bone. As more cartilage is formed, the epiphyseal plate advances, leaving bone behind it. Thus, bone is remodeled by cellular activity. Diaphysis is the region of bone be-tween the epiphysis. The diaphysis forms the middle, cylindrical part of the bone. The metaphysis is the region of bone that lies between the diaphysis and the epiphysis, and it includes the epiphyseal plate.
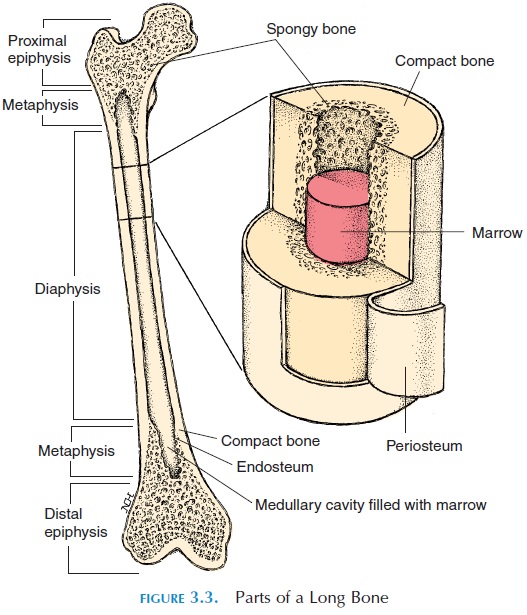
The ends of long bones, adjacent to the joint, are covered with hyaline cartilage - articular cartilage. The articular cartilage absorbs shock and reduces fric-tion in joints. The inner region of long bones houses the medullary or marrow cavity.
In children this cavity is filled with red bone marrow (where blood cells are formed). In older individuals, the red bone marrow is replaced by yellow marrow that is largely made up of adipose tissue. The medullary cavity is lined by the endosteum membrane. It contains containing bone-forming cells (osteogenic cells and osteoblasts).
Bone continues to lengthen rapidly during puberty and stops in adulthood. However, bone deposition and resorption continues throughout life and is mod-ified by diet and endocrine, mechanical, chemical, and psychological factors.
Effect of Diet on Bone
For proper bone formation, there must be adequate protein, calcium, and phosphorus, among others, es-pecially at rapid growth phases such as childhood, adolescence, pregnancy, and lactation. Because bone is also a calcium reservoir, if demands are increased, calcium is removed from the bones to meet those needs and the bones can get weaker. Small quantities of fluoride, magnesium, manganese, and iron are also needed. Vitamin C is needed for proper collagen fiber development. Other vitamins, such as vitamin A, B12, and K, are needed for protein synthesis and os-teoblastic activity.
Effect of Hormones on Bone
Three hormones are important in maintaining blood levels of calcium. This implies that they affect the mineralization of bone in the process. Parathormone, from the parathyroid gland, and vitamin D increase the blood levels of calcium while the hormone calcitonin, from the thyroid gland, de-creases the levels. In bone, parathormone and vita-min D increase osteoclastic activity and resorption of bone and decrease excretion of calcium by the kid-neys and increase absorption in the gut. Calcitonin does the opposite; if dietary calcium is inadequate, bone resorption occurs.
In addition to these hormones, growth hormone, thyroid hormone, insulin, and sex hormones are all required for proper bone formation.
Effect of Mechanical Factors on Bone
The plasticity of bone can be illustrated in many ways. Bones of athletes are stronger and denser as com-pared with sedentary individuals. Similar to other tis-sue that atrophy with disuse, bone becomes weaker and less dense when not stressed. Conversely, exces-sive stress placed on one or more bones makes those bones alone stronger and denser. Hence, posture, muscle tone, and weight can all affect the remodeling process.
TYPES OF BONES
The bones of the body are classified, according to shape, as long bones, short bones, flat bones, and irregular bones (see Figure 3.4). Long bones, as thename suggests, are long, with the length being greater than the width. The femur or thighbone, the humerus of the arm, metacarpals, metatarsals, and phalanges are a few examples.
Short bones are almost equal in length, width,and height. Most of the carpals—the small bones lo-cated in the wrist (except pisiform, sesamoid bone)— and most of the tarsals—the small bones in the ankle region (except calcaneus, irregular bone)—are good examples of short bones.
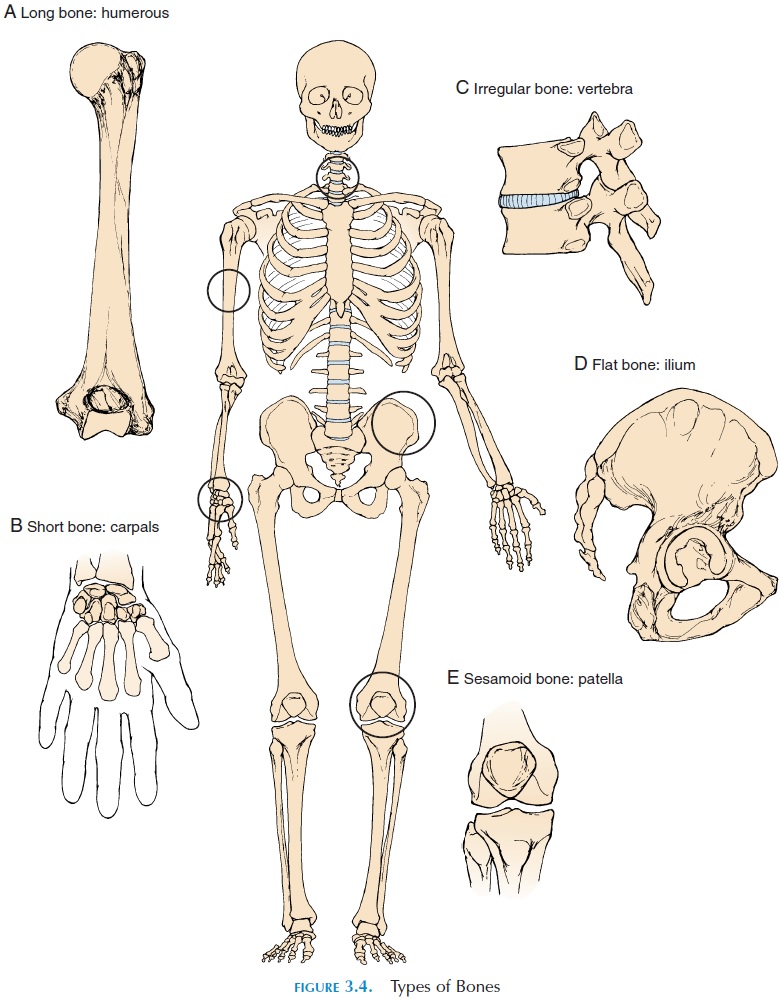
Flat bones are broad and thin with a flattenedand/or curved surface. The shoulder blade (scapula), some of the skull bones, ribs, and breastbone (ster-num), are all examples of flat bone. Their thin, broad area helps protect inner organs and/or provide surface area for muscle attachment. Flat bones contain the red bone marrow in which blood cells are manufactured.
Irregular bones are those in various shapes andsizes. The facial bones and vertebrae are all examples of this type. Small, irregularly shaped bones, called sutural orwormian bones, are found where two ormore other bones meet in the skull. The number, size, and shape vary by individual.
Rarely, small, flat, round bones develop inside ten-dons. These bones are called sesamoid bones. The patella is a sesamoid bone found in all individuals. Other sesamoid bones are often found around the knee joint or the joints of the hands or feet. Sesamoid bones help reduce friction and stress on tendons and may also help to change the direction of tension placed on the tendon.
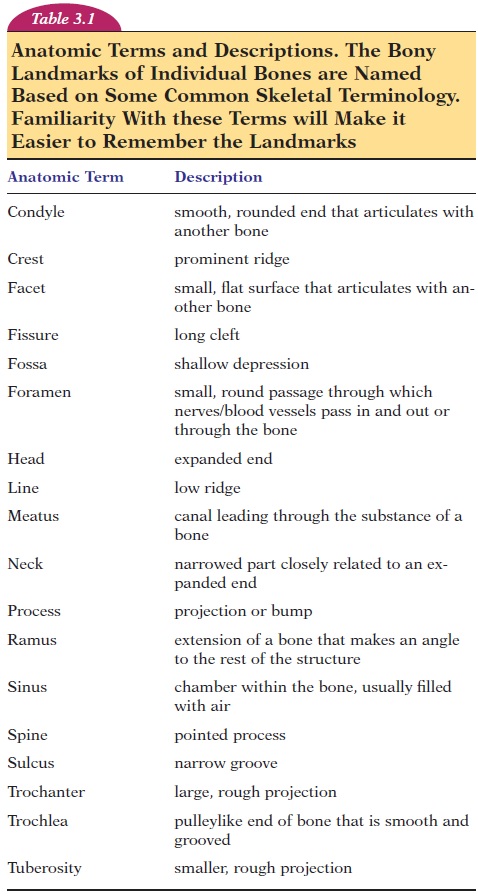
To examine joints and learn about muscles and the movements they produce, the names of the bones of the body and the anatomic landmarks of each bone must be looked at in greater detail (see Table 3.1).
Related Topics