Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Skeletal System and Joints
Joint Classifications
Joints
Although the bones provide the solid structure to which muscles are attached, it is the presence of joints, or articulations, which enable the body tomove. The way two or more bones join with each other determines the type of movement and the range of motion.
To understand the possible movements of a joint, the joints have been classified in many ways.
JOINT CLASSIFICATIONS
Joints are classified according to the structure and function (i.e., how much movement they allow). Structurally, they are classified as fibrous (has fi-brous connective tissue between the bones), carti-laginous (has cartilage between bones), and synovial (has a cavity with fluid separating the bones). Func-tionally, they are classified assynarthrosis (immov-able joint), amphiarthrosis (slightly movable joint), and diarthrosis (freely movable joint). The func-tional classification is described below. Note that thefibrous and cartilaginous joint types fall under synarthrosis and amphiarthrosis and synovial joint type falls under diarthrosis of the functional classifi-cation. A joint in singular form is spelled with –is, and with –es in plural form (e.g., synarthrosis [singu-lar]; synarthroses [plural]).
Synarthrosis
In some parts of the body, joints exist where the movement is minimal or not possible. This type of joint is known as synarthrosis (synonym, together) or immovable joint. The region where the two bones meet may have fibrous tissue or cartilage. An exam-ple of an immovable joint is where the different bones of the skull meet. The location of the joint can be identified in infants before the skull bones fuse. The subtype of joint seen in the skull is known as su-ture. Synarthrosis is also seen in the jaw, where the tooth is embedded into the socket or alveolus. Dense fibrous tissue, as in the skull, connects the tooth to the socket. This subtype of joint is gomphosis.
Another category of joint under synarthrosis is seen between parts of a single bone—between the epiphysis and diaphysis separated by the cartilagi-nous epiphysial plate, before the ossification centers fuse. Another example is found between the ribs and the sternum. The type of synarthrosis with cartilage in the joint area is known assynchondrosis.
The bones in some parts of the body, as in certain bones of the skull, fuse, with no trace of the joint. This type of joint is known as synostosis. An exam-ple of synostosis is the fusion of the two sides of the frontal bone in infancy.
Amphiarthroses
Certain joints allow slight movement. These are known as amphiarthroses, or slightly movable joints. These joints, while allowing some slight movement, are stronger than those joints that allow free movement. In one subtype, syndesmosis, the two bones are connected by ligaments. For example, the tibia and the fibula of the leg and the ulna and radius of the arm are joined together by the tough interosseous ligament. In an-other subtype, symphysis, the two bones covered with hyaline cartilage is joined by a pad of fibrocartilage. The joint between the two pubic bones (pubic symph-ysis), the joint between the body of the vertebrae (bones separated by the intervertebral disks), and the joint between the manubrium and body of sternum are examples of symphysis. Note that the symphyses are present in the midline of the body.
Diarthroses
Most joints of the body are freely movable. These are known as diarthroses, or freely movable joints.
Because the articular surfaces of the joints are sep-arated by synovial fluid and synovial membrane lines the articular cavity, these joints are also known as synovial joints.
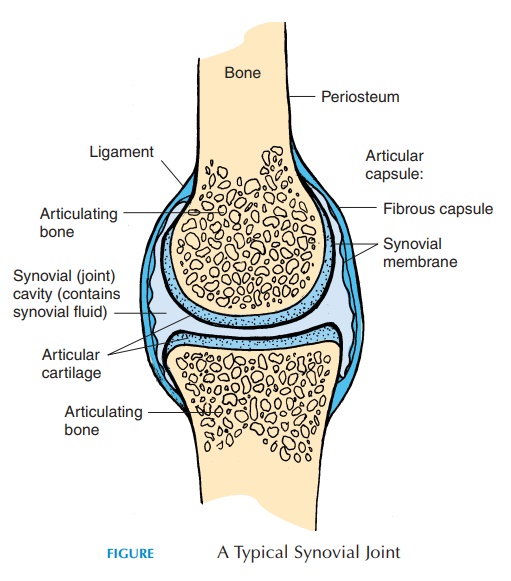
Structure of a Typical Synovial Joint
The structure of a typical synovial joint is shown in Figure 3.32. The synovial joint is surrounded by a thick connective tissue joint or articular capsule. The capsule runs across the bones that articulate with each other and becomes continuous with the perios-teum. The capsule may be described as having two layers—the external fibrous layer and the internalsynovial layer, also referred to as the synovial mem-brane. The fibrous layer is made of dense, irregularconnective tissue that is flexible enough to allow movement and strong enough to prevent dislocation of the bones. This layer is penetrated by blood vessels and nerves. In some joints the capsule may be thick-ened along lines of stress or reinforced with separate thick connective tissue called ligaments.
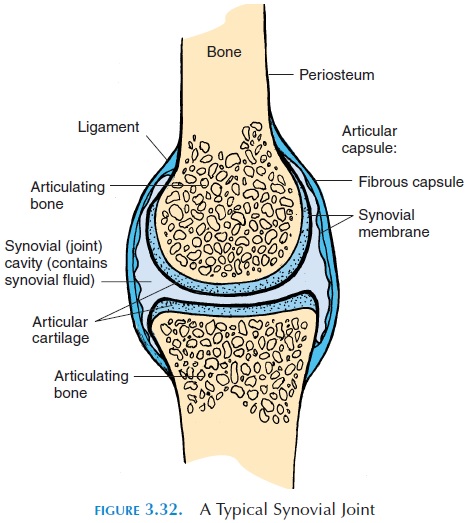
The synovial membrane is present along the in-ner surface of the capsule, forming a closed sac called the joint or synovial cavity. Its inner layer consists of specialized squamous or cuboidal cells that help manufacture the synovial fluid present in the cavity. This innermost layer is surrounded by a network of connective tissue that contains blood vessels, nerves, and, in some joints, fat. The accumulation of adipose tissue is known as articular fat pads. The synovial membrane covers tendons that pass through certain joints. For example, it covers the popliteal tendon in the knee and it covers the tendon of the long head of the biceps in the shoulder. It does not cover that part of the joint where cartilage is present.
The surfaces of the bones that form the joint do not come in direct contact with each other because they are lined by the articular cartilage. This hyaline cartilage is smooth, following the contours of the bone surface. It does not have a blood supply, nor is it innervated. It is nourished by synovial fluid and diffusion from small blood vessels that supply the bone. The cartilage, along with the synovial fluid, helps reduce friction between the moving surfaces. Damage to the articular cartilage can reduce easy movement of the surfaces over each other and limit the range of motion.
The synovial fluid in the joint cavity resembles the interstitial fluid but contains proteoglycans secreted by the fibroblasts of the synovial membrane. The fluid is, therefore, thick and viscous. Synovial joints have about 3 mL (0.1 oz) of fluid in the cavity. The synovial fluid serves to (a) lubricate the joint—the fluid reduces the friction between the moving sur-faces of the joint; (b) distribute nutrients and removewastes—the articular cartilage, having no directblood supply, derives most of its nutrients from the synovial fluid and disposes its waste products into it. The synovial fluid is constantly circulating in the joint as it moves, and its composition is maintained by exchange between the fluid and the blood flowing in the capillaries that supply the joint. The produc-tion of synovial fluid is facilitated by the movement of joints; (c) absorb shock—as the joints move, the ar-ticular surfaces are compressed and the fluid helps distribute the pressure evenly across the articular surfaces; and (d) defense—the synovial fluid contains a few white blood cells that remove debris and pre-vent entry of microorganisms.
The synovial joint may have other accessory struc-tures that further strengthen and stabilize the joints.These may be in the form of additional pads of carti-lage, fat, ligaments, tendons, or bursae.
Some joints, such as the knee joints, have addi-tional fibrocartilage interspersed between the articular surfaces inside the synovial cavity. These moon-shaped disks, known as articular disks or meniscus(plural, menisci), alter the shape of the articulating surfaces and/or help channel the synovial fluid.
Some joints have fat pads lined by synovial mem-brane. They protect the articular cartilage and fill the spaces in the joint cavity as the joint moves, akin to packing material.
Ligaments are thick, connective tissue bands thathelp stabilize moving surfaces. Some are thickenings of the joint capsule and known as accessory liga-ments. Accessory ligaments strengthen the joint cap-sule and reduce rotation at the joint. Others are thick bands that lie outside the joint capsule, providing ad-ditional support to the joint and known as extracap-sular ligaments. Others lie inside the synovial joint,preventing movements that may damage the joint and are known as intracapsular ligaments.
Tendons—the thick connective tissue that connectsmuscle to bon—although not part of the joint, help sta-bilize, support, and limit the range of motion of the joint as they pass across it. Some tendons have connec-tive tissue sheaths filled with synovial fluid and lined with synovial membrane, surrounding them where they lie directly over bone. The sheaths help reduce fric-tion as the tendons go through bony or fibrous tunnels. These sheaths are known as synovial tendon sheaths.
Many joints are surrounded by pockets of synovial fluid-filled cavities in the connective tissue surround-ing them. These cavities, lined by synovial membrane, are bursae(singular, bursa). Bursa may be separate from the joint or connected to the joint cavity. The bursae serve as shock absorbers and also reduce fric-tion between moving structures near the joint. Bursae may be found near tendons, joint capsules, ligaments, muscle, bone, or skin (Figures 3.32 and 3.46).
Check up innervation of joints and add
All joints are supplied by branches of nerves that innervate skeletal muscles close to the joint. Sensory nerves supplying the joint respond to stretch, pain, and degree of movement and convey the information to the spinal cord and brain for a suitable response. The receptors are located in the articular capsule and ligaments.
The joints receive their blood supply from sur-rounding arteries. The articular cartilage does not have a blood supply. Instead, it gets nutrients from the synovial fluid. Waste products are removed from the joints by veins.
Related Topics