Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Skeletal System and Joints
Joints of the Pelvic Girdle and Lower Limbs
Joints of the Pelvic Girdle and Lower Limbs
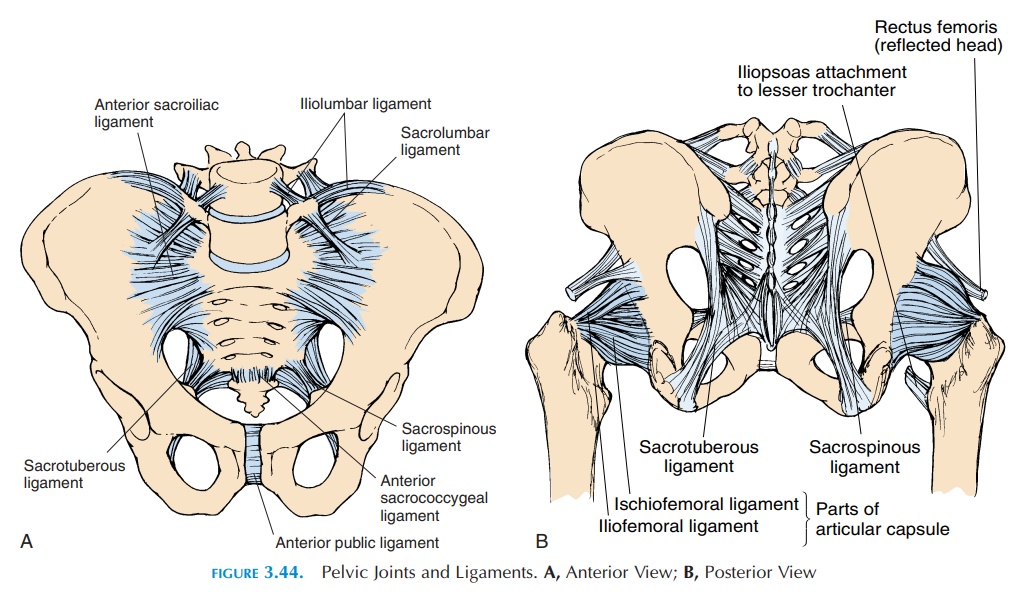
The joints of the pelvic girdle (see Figure 3.44) must be considered in conjunction with the joints of the lower lumbar region and hips because dysfunction of any one structure can affect the function of all others. For example, fusion of the lower lumbar vertebrae, differ-ences in leg length, and stiffening of any of these joints can result in pain and stress on other structures.
Therefore, the structures of this region are often referred to as the lumbopelvic complex, which in-cludes the fourth and fifth lumbar joints, the sacroil-iac joints, sacrococcygeal joint (symphysis), the hip joints, and the pubic symphysis.
A major function of the pelvic girdle is to transmit the weight of the upper body to the lower limbs and forces from the lower limb to the upper body. The sacroiliac joints are important for walking by absorb-ing forces from the leg and protecting the disks.
SACROILIAC JOINT
In osteopathic medicine, the sacroiliac joint is con-sidered as two joints—the sacroiliac joint (where the sacrum moves in relation to the ilium) and iliosacral joint (where the ilium moves in relation to the sacrum). This is so because the sacrum is associated with the spine and helps transmit forces from above to the pelvis, and the ilium is closely associated with the lower limb and transmits forces upwards.
Articulating Surfaces and Type of Joint
The two synovial joints between the medial surface of the ilium and the lateral aspect of the upper sacral vertebrae are L-shaped when viewed laterally. The ar-ticular surfaces are covered with cartilage and marked by elevations and depressions that fit each other and make the joint stronger.
Ligaments
The ligaments that bind the sacrum to the ilium withstand the major forces through the sacroiliac joints. They form a network of fibrous bands. Many ligaments—iliolumbar, sacrolumbar, sacroiliac (an-terior and posterior), sacrotuberous (sacrum to is-chial tuberosity), and sacrospinous—are found around the joints (Figure 3.44). Of these, the iliolum-bar, which extends from the transverse process of the 5th vertebrae to the posterior iliac crest, is the most important as it stabilizes the 5th vertebrae on the sacrum. In addition, the muscles adjacent to the joint—gluteus maximus, gluteus minimus, piriformis, latissimus dorsi, quadratus lumborum, and iliacus— have fibrous attachments that blend with the liga-ments and make the joints even stronger.
Possible Movements and Range of Motion
The movements of this joint are limited, but even this limited movement is important. The main function of this joint is to serve as a shock absorber. The move-ment of the sacrum is described as flexion (nutation) and extension (counter-nutation). During flexion the sacral promontory moves anteriorly and inferiorly with the apex moving posteriorly, while the iliac bones approximate and the ischial tuberosities move apart. Such a movement occurs when walking and when bending forward (flexion) and backward (exten-sion). During walking, the movement of the sacrum is determined by the forces from above, while the move-ment of the ilium is determined by the femur.
Muscles
Though this joint is surrounded by strong muscles, none play a direct part in moving the sacrum. Sacral movement is a result of the pull of forces through lig-aments and gravity. By pulling on the ilia, the muscles in the vicinity have an indirect effect on the sacrum.
There are 35 muscles attached to the sacrum or hipbones and, together with the ligaments and fascia, they help coordinate movement of the trunk and lower limbs. Problems associated with any of them can result in alteration of the mechanics of the pelvis. The quadratus lumborum, erector spinae, abdominal muscles, rectus femoris, iliopsoas, tensor fascia latae, piriformis, short hip adductors, hamstrings, gluteus maximus, medius and minimus, vastus medialis and lateralis, the pelvic floor muscles are important mus-cles that must be considered in a client with low back pain.
Physical Assessment
When assessing this joint, it is important to take a good history that includes history of trauma and ab-normal stress to the region. Typically, the pain arising from this joint is unilateral, increased by walking, get-ting off the bed, and climbing stairs, etc. Examination of this joint should be done in conjunction with the hip joint and lumbar spine as the pain may be re-ferred to this joint from those areas. Description of in-dividual tests used for assessing this joint is beyond the scope of the book. The gait, posture, alignment of bony structures, difference in leg length, and passive and active movements should be tested, and treat-ment aimed at normalizing the stresses on the lum-bopelvic complex should be based on the findings.
THE HIP JOINT
Articulating Surfaces and Type of Joint
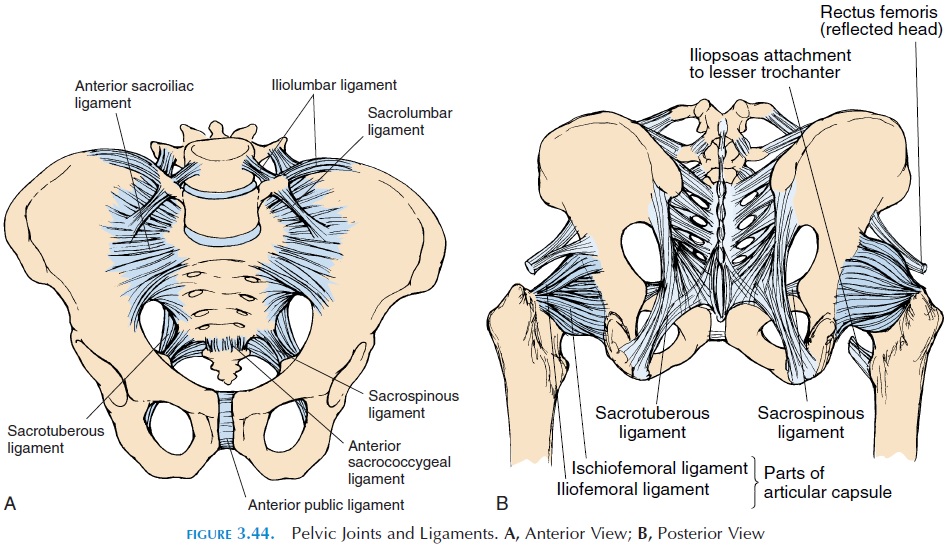
The hip joint, also referred to as the acetabulofemoral or iliofemoral joint, is one of the most stable joints be-cause the articular surfaces of the rounded head of the femur and the acetabulum of the pelvis fit well into each other. The acetabulum is further deepened by the fibrocartilage (acetabular labrum) located in the ac-etabulum. In addition to shape of the articular surface, the hip joint, similar to the shoulder, has supporting ligaments (see Figure 3.45).
Ligaments and Bursa
The thick capsule is reinforced by strong ligaments. The iliofemoral ligament is a thick band that runs between the anterior inferior iliac spine and the in-tertrochanteric line of the femur. This ligament pre-vents excessive internal and external rotation. When standing, this ligament is twisted and pulled taut and results in “locking” of the joint, allowing the person to stand with little muscle action. The pubofemoralligament extends from the pubic portion of the ac-etabular rim to the inferior portion of the neck of the femur. The ischiofemoral ligament runs between
The transverse acetabular liga-ment runs between the gap in the inferior margin ofthe acetabular labrum. Another ligament, the liga-mentum teres, is located inside the joint capsule andruns between the acetabular notch and a small de-pression (fovea capitis) located in the femoral head.
A few bursae surround the hip joint. The il-iopectineal bursa lies on the anterior aspect of thehip joint, deep to the iliopsoas muscle, as it crosses the joint. It may communicate with the joint cavity of the hip joint. The trochanteric bursaelie over the greater trochanter, deep to the gluteus maximus, re-ducing friction between the bone and muscle.
Possible Movements
The hip permits flexion, extension, adduction, abduc-tion, medial rotation, lateral rotation, and some cir-cumduction.
Range of Motion
Abduction, 45–50°
Adduction, 20–30°
External/lateral rotation, 45°
Internal/medial rotation, 35°
Flexion, 135°
Extension, 30°
Muscles
The action of most muscles around the hip can be de-termined from the location. The flexor muscles are located in the anterior quadrant, the extensors in the posterior quadrant, the adductors in the medial, and the abductors in the lateral quadrant.
Muscles that flex the hip:
Primary flexor
Iliopsoas
Secondary flexors
Rectus femoris Sartorius
Muscles that extend the hip:
Primary extensor
Gluteus maximus
Secondary extensor
Hamstrings
Muscles that abduct the hip:
Primary abductor
Gluteus medius
Secondary abductors
Gluteus minimus Tensor fascia lata
Muscles that adduct the hip:
Primary adductor
Adductor longus
Secondary adductors
Adductor brevis Adductor magnus Pectineus Gracilis
Muscles that rotate the hip laterally: Gluteus maximus
Gluteus medius and minimus (posterior fibers) Muscles that rotate the hip medially:
Adductor magnus, longus, brevis
Gluteus medius and minimus (anterior fibers) Iliopsoas
Physical Assessment
Inspection
The gait should be observed as the person enters the room. It is preferable to have the patient’s body ex-posed waist down. When standing normally, the an-terior superior iliac spine should be level with a slight anterior curvature of the lumbar spine. Absence of the lumbar lordosis may indicate spasm of the mus-cles. Weakness of the abdominal muscles may exhibit an abnormally increased lordosis. Look for muscle wasting and body asymmetry.
Palpation
Bony prominences: Various bony prominences can be easily palpated. These are the anterior superior iliac spines, iliac crest, greater trochanter, and pubic tu-bercles anteriorly. Posteriorly, the posterior superior iliac spine and the ischial tuberosity can be palpated.
Other structures: The inguinal ligament, which runs between the anterior superior iliac spine and the pubic tubercle, marks part of the route taken by the male testis as it descends into the scrotum. Bulges in this region may indicate an inguinal hernia. The femoral artery pulsation can be felt just inferior to the inguinal ligament. The femoral vein lies just me-dial to the artery. Tenderness over the sciatic nerve as it emerges from the sacral region can be palpated.
The active and passive range of motion of the hip should be tested as well, together with discrepancies between the two legs.
THE KNEE JOINT
Articulating Surfaces and Type of Joint
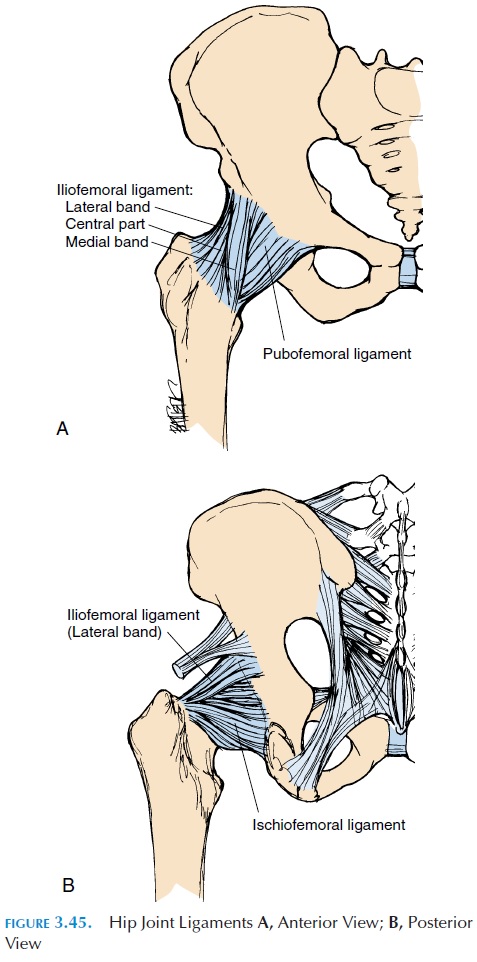
The knee joint, or tibiofemoral joint, (see Figure 3.46) is one of the largest, most complex, and most frequently injured joints in the body and a thorough knowledge of its anatomy is important. It is a hinge joint. The fibula does not articulate with the femur and comes in con-tact only with the lateral surface of the tibia.
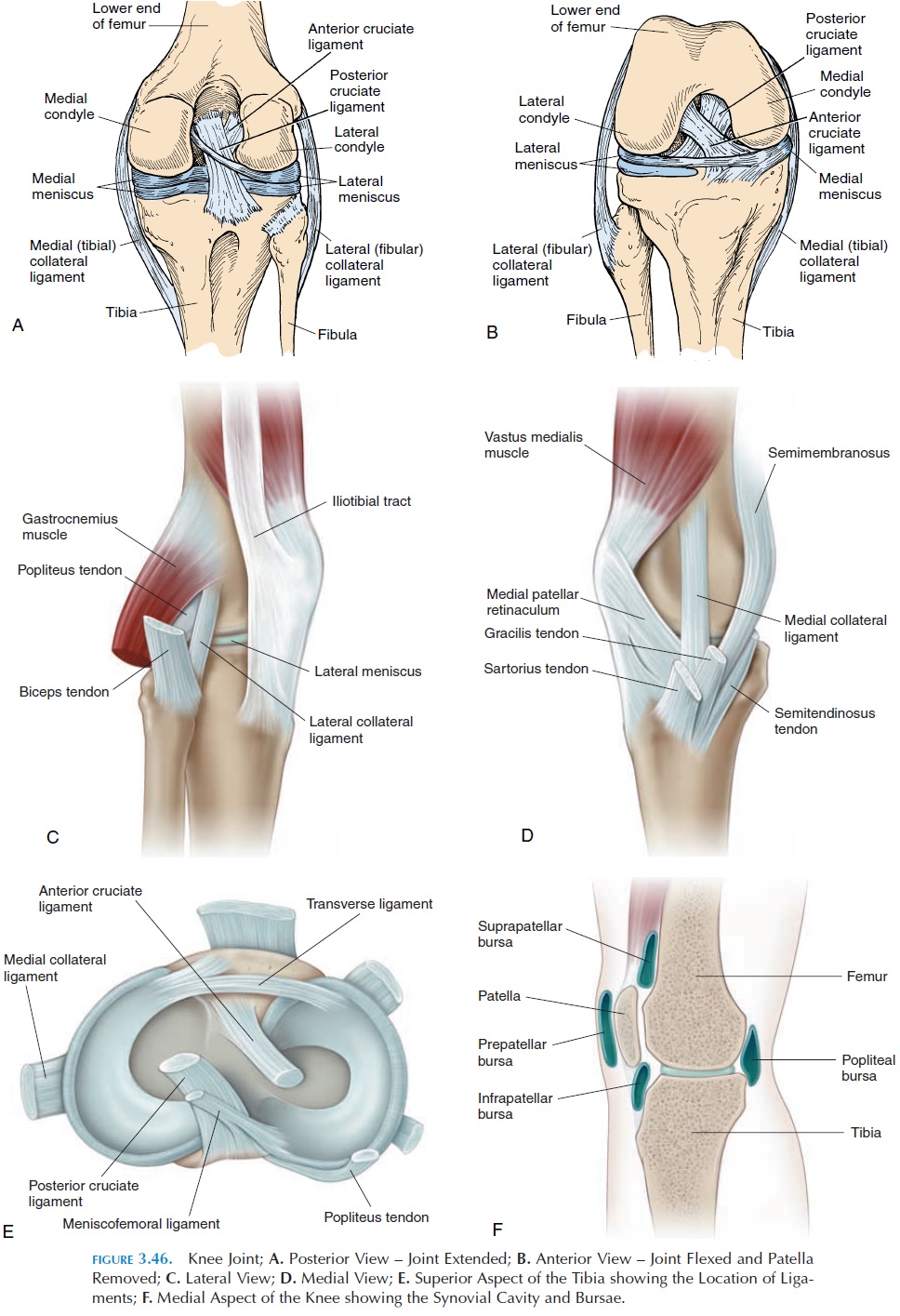
The lower end of the femur, with its condyles and deep fossa between them, articulates with the flat up- per surface of the tibia. Numerous ligaments, carti-lages, and tendons help stabilize this joint. The articu-lating surface is deepened by the presence of two half-moon–shaped fibrocartilage disks—the medial and lateral meniscus—located on the tibia (Figure 3.46E).The menisci also serve as shock absorbers, spreading the stress on the joint over a larger joint surface and helping lubricate the joint and reduce friction.
Ligaments
The knee joint has ligaments located inside and outside the joint capsule. Inside the joint, there are two liga-ments that run anteroposteriorly, preventing excessive forward and backward movement. The anterior cruci-ate ligament runs from the anterior part of the tibia tothe medial side of the lateral femoral condyle. It pre-vents excessive forward movement (hyperextension) of the tibia. The posterior cruciate ligament extends su-periorly and anteriorly from the posterior aspect of the tibia to the lateral side of the medial condyle. It pre-vents the tibia from slipping backward and, with the popliteus muscle, it prevents the femur from sliding anteriorly over the tibia in a squatting position.
The patellar tendon—a thick, fibrous band that extends from the patella to the tibial tuberosity—is actually an extension of the quadriceps tendon that stabilizes the joint anteriorly. Thin fibrous bands— patellar retinaculum—extend from the side of thepatella to the tibial condyles. Posteriorly, the capsule is thickened to form the oblique popliteal ligament, an extension of the semimembranous tendon. An-other thickening—the arcuate popliteal ligament— runs from the posterior fibular head to the capsule.
Medially, the medial collateral ligament, or the tibial collateral ligament, runs from the medial epi-condyle of the femur to the medial surface of the tibia. This ligament helps stabilize the joint medially and prevents anterior displacement of the tibia on the femur.
Another ligament—lateral collateral ligament, or the fibular collateral ligament, runs from the lateral epicondyle of the femur to the head of the fibula, sta-bilizing the joint laterally. Other small ligaments ex-ist. The coronary ligament attaches the menisci to the tibial condyle, the transverse ligament connects the anterior portions of the medial and lateral menisci, and the meniscofemoral ligament runs posteriorly, joining the lateral menisci to the medial condyle of the femur.
In addition to the support provided by the liga-ments, the joint is stabilized medially by the pes anser-inus tendons (semitendinosus, gracilis, and sartorius)and the semimembranosus tendon. The posterolateral region is supported by the biceps femoris tendon, and the posterior aspect is reinforced by the origins of the gastrocnemius muscles and the popliteus muscles.
Bursae
The knee joint is surrounded by numerous bursae. The largest is the suprapatellar bursa, or quadri-ceps bursa, an extension of the joint capsule that al-lows movement of the thigh muscles over the lower end of the femur. Subcutaneous bursae—the subcu-taneous or superficial prepatellar and infrapatel-lar bursa and the deep infrapatellar bursa—sur-round the patella. A large fat pad, the infrapatellar fat pad, exists deep to the patella tendon. The fat pad is lined on the deep surface by synovial membrane and is thought to help lubricate the joint as it deforms during flexion and extension of the knee.
In addition to the above, bursae exist in the popliteal fossa—popliteal bursa—and near the gas-trocnemius—the gastrocnemius bursa. The semi-membranous bursa,which lies deep to the semi-membranosus tendon and the medial origin of the gastrocnemius muscle, often communicates with the joint. Other bursae may exist between the pes anser-inus and the iliotibial band.
Possible Movements
The knee joint allows flexion (with an associated glide), extension (with an associated glide), and in-ternal and external rotation. Active rotation of the knee occurs only when the knee is flexed.
Range of Motion
Flexion, 135°
Extension, 0°
Internal rotation, 10°
External rotation, 10°
Muscles
Muscles that flex the knee:
Hamstrings: semimembranosus, semitendinosus, biceps femoris
Muscle that extends the knee:
Primary extensor
Quadriceps
Muscles that rotate the knee medially: Semitendinosus Semimembranosus
Muscle that rotates the knee laterally: Biceps femoris
Physical Assessment
Inspection
The gait of the individual must be closely watched. Identify abnormal swellings and asymmetry of mus-cles. The knee should be fully extended while standing.
Palpation
Many parts of the bones can be easily palpated in and around the knee. The medial and lateral femoral condyle, the head of the fibula and the patella, and others may be palpated. The muscles and tendons in and around the joint should be palpated for tender-ness. Enlarged bursae (a common ailment) can be felt as a boggy, soft swelling. Tenderness in the joint margins may be a result of tears in the medial and lateral meniscus. The medial and lateral collateral ligaments are also easily palpated. The insertion of the tendons of the sartorius, gracilis, and semitendi-nosus can be palpated on the medial aspect of the joint. The iliotibial tract, a thick fibrous band, runs on the lateral aspect of the knee joint.
In the popliteal fossa, the pulsation of the popliteal artery can be felt.
The stability of the joint must be tested by check-ing the collateral and cruciate ligaments. The range of motion should also be tested actively and passively.
TIBIOFIBULAR JOINT (PROXIMAL AND DISTAL)
The superior or proximal tibiofibular joint is a plane synovial joint formed by the head of the fibula and the posterolateral surface of the tibia (see Figure 3.47). The synovial cavity is often continuous with the knee joint, allowing slight superior and inferior glide and anteroposterior glide and rotation of the fibula.
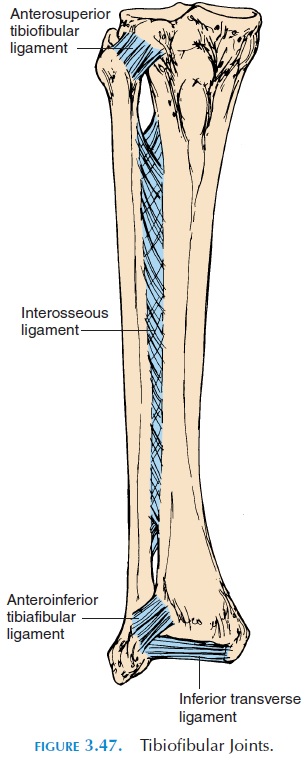
The tibia and fibula are bound together by the in-terosseous membrane that separates the leg into an-terior and posterior compartments.
The inferior tibiofibular joint is a syndesmosis formed by the articulation of the fibula with the lat-eral aspect of the distal end of the tibia. The joint is reinforced by the anterior and posterior tibiofibular ligaments.
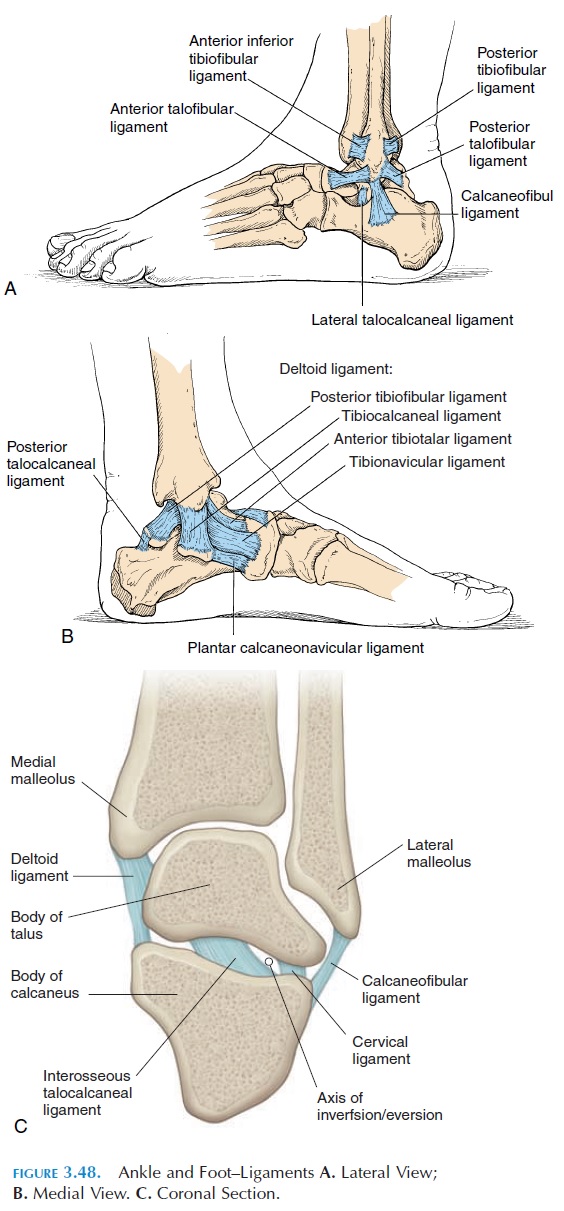
THE ANKLE JOINT AND JOINTS OF THE FOOT
Articulating Surfaces and Type of Joint
The ankle joint (see Figure 3.48) is formed by the dis-tal end of the tibia, fibula, and the superior surface of the talus. This joint is also known as the talocrural joint. It is a hinge joint with the lateral and medialaspect of the capsule thickened to form ligaments.
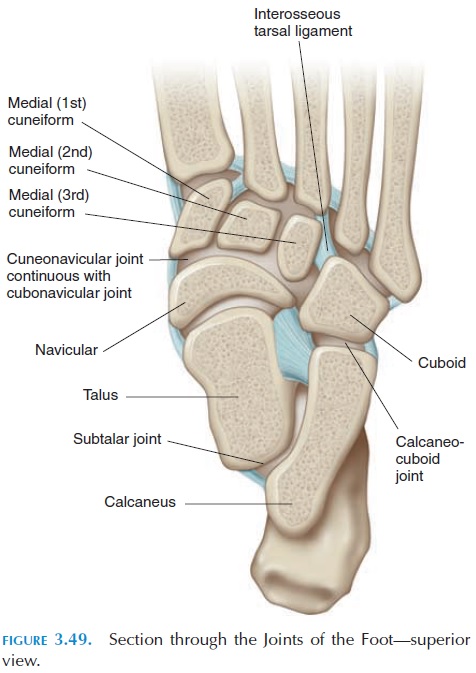
Other articulations (see Figure 3.49) occur between the talus and calcaneus (subtalar joint); between the tarsal bones (midtarsal joints) and talocalcaneonav-icular and calcaneocuboid joints; between the ante-rior tarsals (anterior tarsal joints) and the cubonav-icular , cuneonavicular, cuneocuboid, and intercuboid joints; between the tarsals and the metatarsals (tar-sometatarsal joints); between the metatarsal andphalanges (metatarsophalangeal joint); and be-tween the phalanges (the proximal anddistal inter-phalangeal joints).
Ligaments
The medial ligament, or the deltoid ligament, is a thickening of the medial fibrous capsule that attaches the medial malleolus to the navicular, calcaneus, and talus bones. The calcaneofibular ligament extends from the lateral malleolus to the calcaneus. Anteri-orly and posteriorly, ligaments extend from the lat-eral malleolus to the talus to form the anteriortalofibular (most frequently injured) and posterior talofibular ligaments. The various ligaments pre-vent tilt and rotation of the talus and forward and backward movement of the leg over the talus.
Possible Movements
The ankle allows dorsiflexion and plantar flexion. However, the subtalar joint and tarsal joints allow further movement. Eversion and inversion is possible at the subtalar joint. The foot can be adducted and abducted at the midtarsal joints. The metatarsopha-langeal joints and interphalangeal joints are hinge joints, allowing flexion and extension of the toes.
Range of Motion
Dorsiflexion, 20°
Plantar flexion, 50°
Inversion and eversion, 5°
Adduction, 20°
Abduction, 10°
Flexion (toes), 45°
Extension, 70–90°
Muscles
Muscles that cause plantar flexion:
Primary plantar flexors
Gastrocnemius
Soleus
Secondary plantar flexors
Tibialis posterior
Flexors of the toes
Peroneus longus and brevis
Muscles that cause dorsiflexion:
Tibialis anterior
Peroneus tertius
Extensors of the toes
Muscle that inverts the foot:
Tibialis anterior and posterior
Muscle that everts the foot:
Peroneus longus, brevis, and tertius
Physical Assessment
Inspection
The external appearance of the shoe and foot should provide information. The alignment of the toes and the shape of the foot and arches should be inspected. The color of the skin and presence of swelling should also be noted.
Palpation
The bones of the foot and ankle are easily palpated. Some bony prominences that can be located are the malleoli, talus, calcaneus, and the metatarsal and phalanges. The deltoid ligament is also palpable infe-rior to the medial malleolus. The long saphenous vein, if dilated may be visible just anterior to the me-dial malleolus. Both active and passive range of mo-tion should be tested at the various joints.
ARCHES OF THE FOOT
The foot has three major arches that help distribute the weight of the body between the heel and the ball of the foot during standing and walking. Two longitudi-nal—themedial and the lateral longitudinal arch— and one transverse—the transverse arch—exist. The shape of the arch is maintained by ligaments, the ten-dons attached to the foot, and the configuration of the bones. The medial arch is formed by the calcaneus, talus, navicular, cuneiforms and the medial three metatarsal bones. The lateral arch is formed by the calcaneus, cuboid, and the two lateral metatarsals. The transverse arch is formed bby the cuboid and cuneiform bones.
Related Topics