Chapter: Ophthalmology: Cornea
Noninfectious Keratitis and Keratopathy
Noninfectious Keratitis and Keratopathy
This category encompasses a wide variety of
corneal disorders, some of which, such as keratoconjunctivitis sicca, occur
very frequently. Causesinclude:
❖ Inflammations (blepharitis and
conjunctivitis).
❖ Injuries (rubbing the eyes, foreign bodies
beneath the upper eyelid, con-tact lens incompatibility, exposure to intense
ultraviolet irradiation).
❖ Age-related changes (senile ectropion with
trichiasis; spastic entropion; keratoconjunctivitis sicca).
❖ Surgery (cataract or glaucoma).
❖ Endogenous factors (facial neuropathy).
❖ Exogenous factors (medications or
preservatives).
Superficial Punctate Keratitis
Definition
Superficial punctate corneal lesions due to
lacrimal system dysfunction from a number causes (see etiology).
Epidemiology and etiology:
Superficial punctate keratoconjunctivitis is avery frequent finding as it can be
caused by a wide variety of exogenous factorssuch as foreign bodies beneath the
upper eyelid, contact lenses, smog, etc. It may also appear as a secondary
symptom of many other forms of keratitis (see the forms of keratitis discussed
in the following section). It can also occur in association with an endogenous
disorder such as Thygeson’s disease.
Symptoms:
Depending on the cause and severity of the
superficial corneallesions, symptoms range from a nearly asymptomatic clinical
course (such as in neuroparalytic keratitis in which the cornea loses its
sensitivity) to an intense foreign body sensation in which the patient has a
sensation of sand in the eye with typical signs of epiphora, severe pain,
burning, and blepharo-spasm. Visual acuity is usually only minimally
compromised.
Diagnostic considerations and differential diagnosis:
Fluorescein dye isapplied and the eye is
examined under a slit lamp. This visualizes fine epithelial defects. The
specific dye patterns that emerge give the ophthalmol-ogist information about
the etiology of the punctate keratitis (Figs. 5.11a – i).
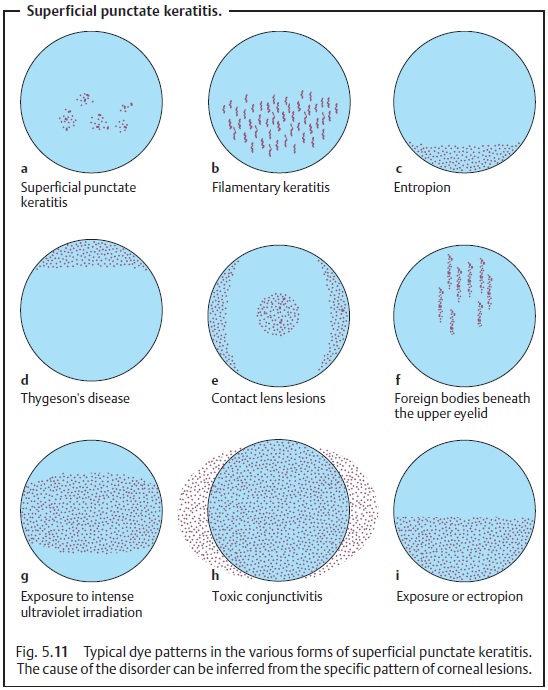
Treatment and prognosis:
Depending on the cause, the superficial cornealchanges will respond rapidly or less so to treatment with artificial tears, whereby every effort should be made to eliminate the causative agents (Fig. 5.11). Depending on the severity of findings, artificial tears of varying viscos-ity (ranging from eyedrops to high-viscosity gels) are prescribed and applied with varying frequency. In exposure keratitis, a high-viscosity gel or ointment is used because of its long retention time; superficial punctate keratitis is treated with eyedrops.
Exposure Keratitis
Definition
Keratitis resulting from drying of the cornea
in the case of lagophthalmos.
Epidemiology:
Exposure keratitis is a relatively frequent
clinical syndrome.For example, it may occur in association with facial
paralysis following a stroke.
Etiology:
Due tofacial
nerve palsy, there is insufficient closure of the eyelidsover the eyeball
(lagophthalmos), and the inferior third to half of the cornea remains exposed
and unprotected (exposure keratitis). Superficial punctate keratitis (see
above) initially develops in this region and can progress to cor-neal erosion
(see Fig. 18.5) or ulcer.
Other causes for exposure
keratitis without facial nerve palsy include:
❖ Uncompensated exophthalmos in Graves’
disease.
❖Insufficient eyelid closure following eyelid
surgery to correct ptosis.
❖Insufficient eye care in patients receiving
artificial respiration on the intensive care ward.
Symptoms:
Similar to superficial punctate keratitis (although
usually moresevere) but unilateral.
Diagnostic considerations:
Application of fluorescein dye will reveal a
typi-cal pattern of epithelial lesions (Fig. 5.11i).
Treatment:
Application of artificial tears is usually not
sufficient where eye-lid motor function is impaired. In such cases, high-viscosity gels, ointmentpackings (for antibiotic
protection), and a watch glass bandage are
required.The watch glass bandage must be applied so as to create a moist
airtight chamber that prevents further desiccation of the eye (see Fig. 2.9). In the pres-ence of persistent
facial nerve palsy that shows no signs of remission, lateraltarsorrhaphy is the treatment of choice. The same applies to
treatment ofexposure keratitis due to insufficient eyelid closure from other
causes (see Etiology).
Poor corneal care in exposure keratitis can
lead to superficial punctate keratitis, erosion, bacterial superinfection with
corneal ulcer, and finally to corneal perforation.
Keratoconjunctivitis Sicca
This is one of the most frequent causes of
superficial keratitis. The syndrome itself is attributable to dry eyes due to
lack of tear fluid.
Neuroparalytic Keratitis
Definition
Keratitis associated with palsy of the
ophthalmic division of the trigeminal nerve.
Epidemiology:
Palsy of the ophthalmic division of the
trigeminal nerve is lessfrequent that facial nerve palsy.
Etiology:
The trigeminal nerve is responsible for the cornea’s sensitivity
toexogenous influences. A conduction disturbance in the trigeminal nerve is
usually a sequela of damage to the
trigeminal ganglion from trauma, radiation therapy of an acoustic
neurinoma, or surgery. It will lead to loss
of corneal sen-sitivity. As a result of this loss of sensitivity, the
patient will not feel any sensa-tion of drying in the eye, and the blinking
frequency drops below the level required to ensure that the cornea remains
moist. As in exposure keratitis, superficial punctate lesions will form
initially, followed by larger epithelial defects that can progress to a corneal
ulcer if bacterial superinfection occurs.
Symptoms:
Because patients with loss of trigeminal
function are free of pain,they will experience only slight symptoms such as a
foreign body sensation or an eyelid swelling.
Diagnostic considerations:
Corneal damage, usually central or
slightlybelow the center of the cornea, may range from superficial punctate
keratitis (visible after application of fluorescein dye) to a deep corneal
ulcer with per-foration. The eye will be red and in extreme cases may be
leaking aqueous humor.
Differential diagnosis:
Corneal ulcer due to herpes virus infection.
Treatment:
This is essentiallyidentical to treatment of exposure keratitis. Itincludes moistening
the cornea, antibiotic protection as prophylaxis against infection, and, if conservative
methods are unsuccessful, tarsorrhaphy.
Primary and Recurrent Corneal Erosion
These changes are generally the result of a
corneal trauma.
Problems with Contact Lenses
Etiology:
These problems occur either withpoorly seated rigid contact lensesthat
rub on the surface of the cornea or from overwearing
soft contact lenses.
If contact lenses are worn for extended
periods of time despite symptoms, severe inflammation, corneal ulceration, and
vascularization of the corneal periphery may result.
Symptoms:
Patients find the contact lenses increasingly
uncomfortable andnotice worsening of their vision. These symptoms are
especially pronounced after removing the contact lenses as the lenses mask the
defect in the corneal epithelium.
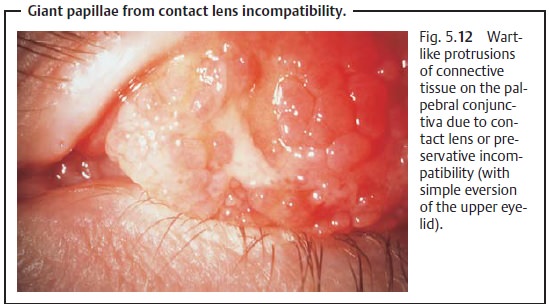
Diagnostic considerations:
The ophthalmologist will detect typical
cornealchanges after applying fluorescein dye (Fig. 5.11e). Keratoconjunctivitis on the superior limbus with formation of
giant papillae, wart-like protrusions of connective tissue frequently observed
on the superior tarsus (Fig. 5.12),
are signs of contact lens or preservative incompatibility.
Treatment:
The patient should temporarily discontinue
wearing the contactlenses, and inflammatory changes should be controlled with
steroids until the irritation of the eye has abated.
Protracted therapy with topical steroids
should be monitored regularly by an ophthalmologist as superficial epithelial
defects heal poorly under steroid therapy. Protracted high-dosage steroid
therapy causes a secondary increase in intraocular pressure and cataract in
one-third of all patients.
The specific ophthalmologic findings will
determine whether the patient should be advised to permanently discontinue
wearing contact lenses or whether changing contact lenses and cleaning agents
will be sufficient.
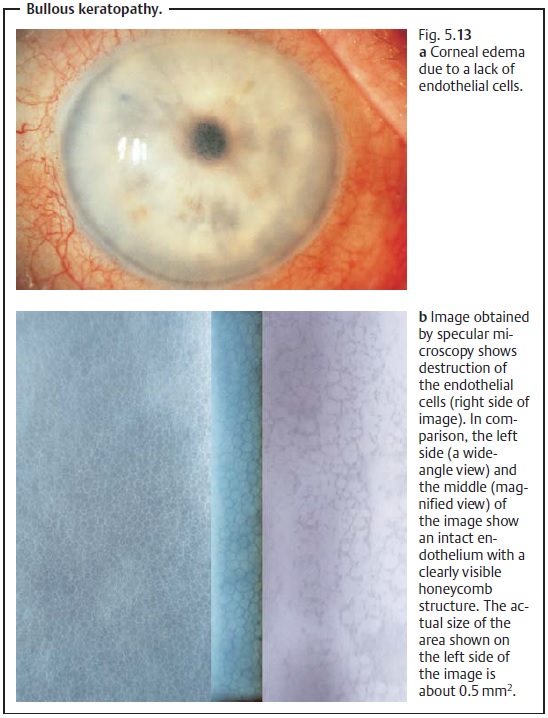
Bullous Keratopathy
Definition
Opacification of the cornea with epithelial
bullae due to loss of function of the endothelial cells.
Epidemiology:
Bullous keratopathy is among the most frequent
indicationsfor corneal transplants.
Etiology:
The transparency of the cornea largely depends
on a functioningendothelium with a high density of endothelial cells (see
Transparency). Where the endothelium has been severely damaged by inflammation,
trauma, or major surgery in the anterior eye, the few remaining endothelial
cells will be unable to prevent aqueous
humor from entering the cornea. This results in hydration of the cornea
with stromal edema and epithelial bullae (see Figs. 5.13a and b). Loss of
endothelial cells may also have genetic causes (see Fuchs’ endothelial
dystrophy).
Symptoms:
The gradual loss of endothelial cells causesslow deterioration ofvision. The patient
typically will have poorer vision in the morning than in theevening, as corneal
swelling is greater during the night with the eyelids closed.
Diagnostic considerations:
Slit lamp examination will reveal thickening
ofthe cornea, epithelial edema, and epithelial bullae.
Differential diagnosis:
Bullous keratopathy can also occur with
glaucoma.
However, in these cases the intraocular
pressure is typically increased.
Treatment:
Where the damage to the endothelial cells is
not too far advancedand only occasional periods of opacification occur (such as
in the morning), hyperosmolar solutions such
as 5% Adsorbonac can improve the patient’s eye-sight by removing water.
However, this is generally only a temporary solu-tion. Beyond a certain stage a
corneal transplant (penetrating
keratoplasty;) is indicated.
Related Topics