Chapter: Ophthalmology: Cornea
Infectious Keratitis
Infectious Keratitis
Protective Mechanisms of the Cornea
As was discussed above, the cornea has certain
defensive mechanisms required because of its constant exposure to microbes and
environmental in-fluences. The mechanisms include:
❖ Reflexive eye closing.
❖ Flushing effect of tear fluid (lysozyme).
❖Its hydrophobic epithelium forms a diffusion barrier.
❖ Epithelium can
regenerate quickly and completely.
Corneal Infections: Predisposing Factors, Pathogens, and Pathogenesis
When certain pathogens succeed in breaching
the corneal defenses through superficial injuries or minor epithelial defects,
the bradytrophic corneal tissue will respond to the specific pathogen with
characteristic keratitis. Predisposing factors that promote inflammation are:
❖ Blepharitis.
❖ Infection of the ocular appendages (for
example, dacryostenosis accom-panied by bacterial infestation of the lacrimal
sac).
❖ Changes in the corneal epithelial barrier
(bullous keratopathy or dry eyes).
❖ Contact lenses.
❖ Lagophthalmos.
❖ Neuroparalytic disorders.❖ Trauma.
❖
Topical and systemic immunosuppressive agents.
Pathogens causing corneal infections may include:
❖ Viruses.❖ Bacteria.
❖ Acanthamoeba.
❖ Fungi.
Pathogenesis: Once these pathogens have invaded the bradytrophic tissuethrough
a superficial corneal lesion, a typical chain of events will ensue:
❖Corneal lesion.
❖ Pathogens invade and colonize the corneal stroma (red eye).
❖ Antibodies will infiltrate the site.
❖ As a result, the cornea will opacify and the
point of entry will open further, revealing the corneal infiltrate.
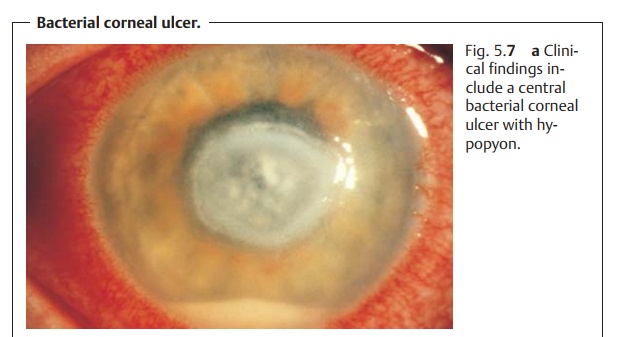
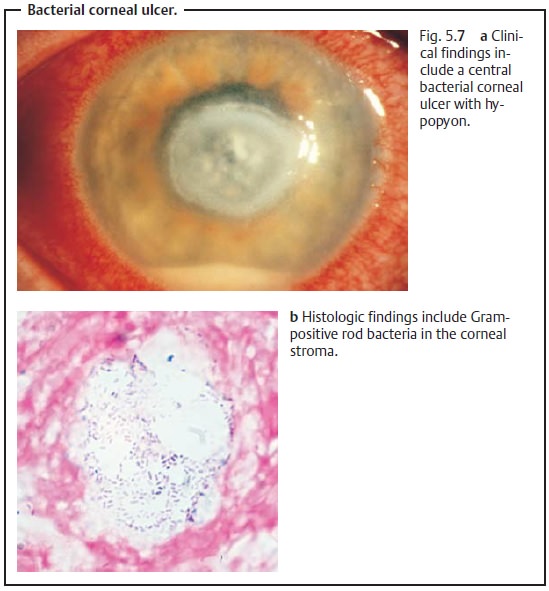
❖ Irritation of the anterior chamber with hypopyon (typically pus willaccumulate on the floor of
the anterior chamber; see Fig. 5.7).
❖ The pathogens
will infest the entire cornea.
❖ As a result the stroma will melt down to
Descemet’s membrane, which is relatively strong. This is known as a descemetocele; only Descemet’s membrane is still intact. Descemet’s membrane
will be seen to protrude anteriorly when examined under a slit lamp.
❖As the disorder progresses, perforation of Descemet’s membrane occurs and the aqueous humor will be seen to leak. This is referred to as a per-forated corneal ulcer and is an indication for immediate surgical interven-tion (emergency keratoplasty;). The patient will notice pro-gressive loss of vision and the eye will be soft.
❖ Prolapse of the iris (the iris will prolapse into the newly created defect)closing
the corneal perforation posteriorly. Adhesion of the iris will pro-duce a white corneal scar.
This sequence of events can vary in speed and
severity. Depending on the voracity of the pathogens and the state of the
patient’s immune system, an infiltrate can form within a few hours or days and quickly progress to a corneal ulcer,
melting of the stroma, and even a descemetocele. This rapidly prog-ressing form
of infectious corneal ulcer (usually bacterial) is referred to as a serpiginous corneal ulcer. It penetrates the cornea particularly rapidly andsoon leads to
intraocular involvement (the pathogens will be active beyond the visible rim of the ulcer). A serpiginous
corneal ulcer is one of the most dangerous clinical syndromes as it can rapidly
lead to loss of the eye.
General Notes on Diagnosing Infectious Forms of Keratitis
Prompt diagnosis and treatment of corneal
infections are crucial in avoiding permanent impairment of vision. The
diagnosis of any type of infectious ker-atitis essentially includes the
following steps:
❖Identifying the pathogen and testing its
resistance. This is done by taking a smear from the base of the ulcer to obtain
sample material and inoculating culture media for bacteria and fungi. Wearers
of contact lenses should also have cultures taken from the lenses to ensure
that they are not the source of the bacteria or fungus.
❖ Slides of smears, unstained and treated with
Gram and Giemsa stains, are examined to detect bacteria.
❖Where a viral infection is suspected, testing
corneal sensitivity is indicated as this will be diminished in viral keratitis.
Related Topics