Chapter: Ophthalmology: Cornea
Cornea: Examination Methods
Examination Methods
Non-ophthalmologists can evaluate the
transparency of the cornea (opaci-ties of the stroma and epithelium suggest
scarring or infiltration of the epithelium), its surface luster (lack of luster suggests an epithelial defect), and
possible superficial corneal injuries
(see Fig. 19.1). A simple ruler
may be used to measure the size of the cornea (see Anatomy), and sensitivity may be tested with a cotton
swab (see Fig. 1.11,).
The ophthalmologist uses instruments to evaluate corneal
morphology and function in greater detail.
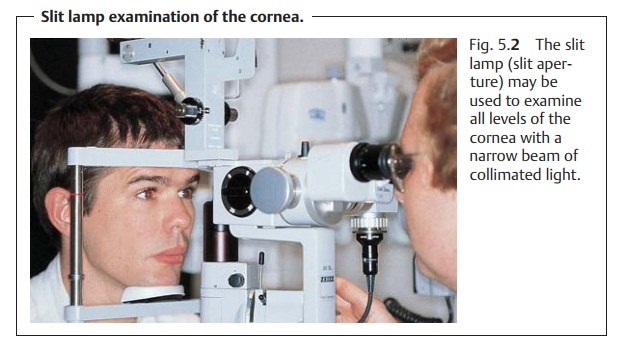
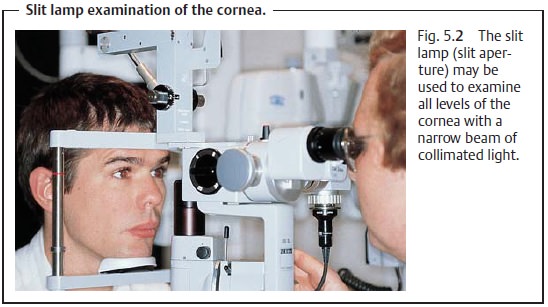
Slit Lamp Examination
The slit lamp is the primary instrument used
in evaluating the cornea. The ophthalmologist chooses between eight and
forty-power magnification for examining all levels of the cornea with a narrow
beam of collimated light (Fig. 5.2).
Dye Examination of the Cornea
Defects in the surface of the cornea can be
visualized with fluorescein or rose bengal solution (in either case, administer
one drop of 1% solution). Since these dyes are not usually absorbed by the
epithelium, they may be used to visualize loss
of epithelium over a wide area (such as corneal erosion) and extremely fine defects (as in
superficial punctate keratitis). Illuminationwith a cobalt blue filter enhances
the fluorescent effect.
These dye methods can reveal corneal epithelial
defects (corneal ero-sion) even without the use of a slit lamp, which is
helpful in examining infants.
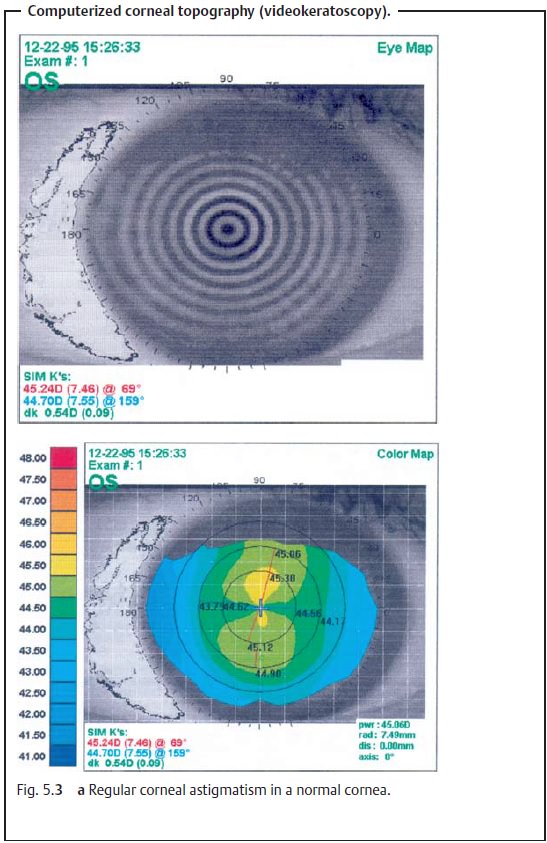
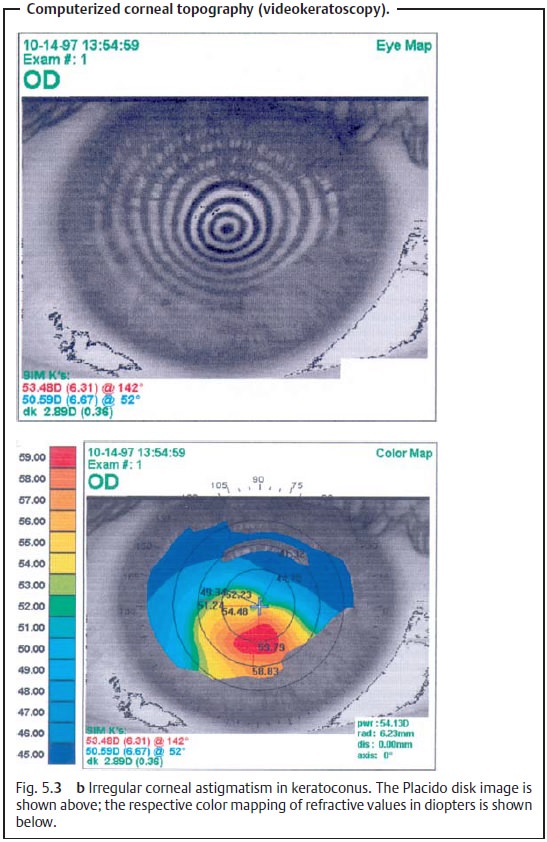
Corneal Topography
The keratoscope (Placido’s disk) permits gross evaluation of
the uniformityof the surface of the cornea. This instrument consists of a round disk
markedwith concentric black and white rings around a central aperture. The
examiner holds the disk in his or her hand and looks through the aperture. The mirror images of the rings on the patient’s
cornea indicate the presence of astigmatism (in which case they appear
distorted). However, this inexact evaluation method lacks the precision
required for modern applications such as refractive surgery. Therefore, the
surface of the cornea is now normally evaluated by computerized corneal topography (videokeratoscopy). In this
examination, the contours of the cornea are measured by a computer in the same
manner as the keratoscope. The refractive values of specific corneal regions
are then represented in a color-coded dioptric map. Bright red, for example,
represents a steep curvature with a high refractive power. This tech-nique
provides a contour map of the distribution of the refractive values over the
entire cornea (Figs. 5.3a and b).
Determining Corneal Sensitivity
Non-ophthalmologists may perform a simple preliminary examination ofcorneal sensitivity with a distended cotton swab (see Fig. 1.11, p. 11). Thisexamination also helps
the ophthalmologist confirm the diagnosis in the presence of a suspected viral
infection of the cornea or trigeminal or facial neuropathy as these disorders
are associated with reduced corneal sensitiv-ity. Ophthalmologists may use an
automatic Dräger esthesiometer for precisetesting
of corneal sensitivity and for
follow-up examinations. This instru-ment can incrementally raise the
sensitivity stimulus. This makes it possible to determine if and how rapidly
corneal sensitivity increases following a cor-neal transplant.
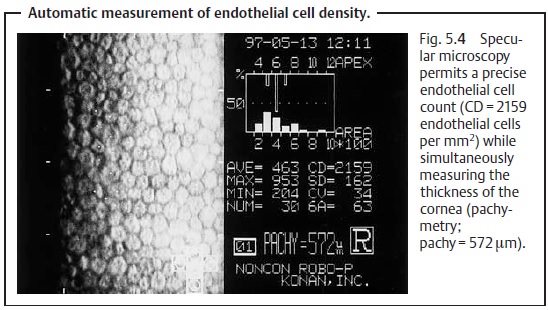
Measuring the Density of the Corneal Epithelium
A sufficiently high density of endothelial cells is very important for the trans-parency of the cornea (see Transparency). Gross estimation of the endothelial cell density is possible for a circumscribed area of the cornea using a slit lamp and indirect illumination. Both the viewing axis and illumination axis are off-set from the visual axis. Precise quantification and morphologic evaluation of endothelial cells over large areas is only possible by means of specularmicroscopy, a technique designed especially for this purpose (Fig. 5.4).
Exact analysis is necessary when the number of cells
appears extremely low under slit lamp examination and the patient is a
candidate for cataract surgery. If exact analysis then verifies that the number
of cells is extremely low (below 300 – 400 cells per mm2), cataract surgery is combined with a corneal trans-plant. This
is done to ensure that the patient will be able to see even after cat-aract
surgery, which sacrifices additional endothelial cells.
Measuring the Diameter of the Cornea
An abnormally large or small cornea
(megalocornea or microcornea) will be apparent from simple visual inspection. A
suspected size anomaly can be easily verified by measuring the cornea with
a ruler. Corneal diameter
may be determined more accurately with calipers (usually done under general anesthesia, see
Fig. 10.21) or with the Wessely keratometer. This is a type of tube with a condensing lens
with millimeter graduations at one end. The examiner places this end on the
patient’s eye and looks through the other end.
Megalocornea in an infant always requires further diagnostic investigationto determine
whether buphthalmos is present. Microcornea may be a sign of congenital defects
in other ocular tissues that could result in impaired func-tion
(microphthalmos).
Corneal Pachymetry
Precise measurement of the thickness of the
cornea is crucial in refractive surgery (see radial keratotomy and correction
of astigmatism, p. 155). Improving refraction often requires making incisions
through 90% of the thickness of the cornea while meticulously avoiding full
penetration of the cornea. There are two pachymetry techniques for measuring
corneal thick-ness with the high degree of precision that this surgery
requires:
❖ Optical pachymetry with a slit lamp and measuring attachment may be performed on the sitting patient.
❖ Ultrasonic pachymetry; this has the advantage of greater precision andcan also be performed
with the patient supine.
Recent developments now permit pachymetry by
means of specular micros-copy (Fig. 5.4).
Confocal Corneal Microscopy
Confocal corneal microscopy is a recently
developed examination technique that makes it possible to scan the cornea over a wide area from the outer layer to
the inner layer. It differs in this regard from slit lamp examination, which
tends to be a focal examination along
a shaft of light perpendicular to the eye. Confocal corneal microscopy
visualizes cell structures at maximum magnifi-cation that cannot be observed in
detail with a slit lamp. These include cor-neal nerves, amebas, and hyphae.
Although not yet routinely used in clinical practice, confocal corneal
microscopy appears to be a promising examination method for the future.
Related Topics