Chapter: Ophthalmology: Cornea
Corneal Degeneration
Corneal Degeneration
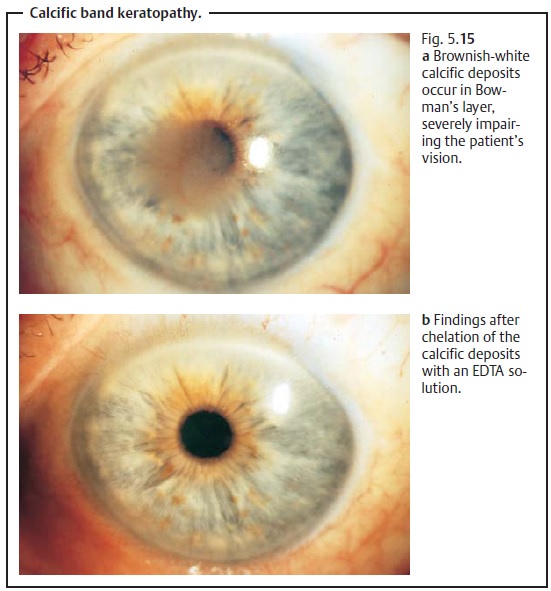
Calcific Band Keratopathy
After many years of chronic inflammation of the anterior chamber (chronic uveitis and keratitis) with shrinkage of the eyeball or in patients with juvenile polyarthritis, calcific deposits occur in Bowman’s layer, causing a transversezone of opacification in the region of the palpebral fissure. The limbusregion will remain clear (Fig. 5.15). This change significantly impairs vision. The opacification can be completely removed and vision restored by chelat-ing the calcifications with a sodium EDTA solution.
Peripheral Furrow Keratitis
This includes a heterogeneous group of disorders in terms of morphology andetiology.
All are noninfectious and lead tothinning and melting of theperipheral cornea that may progress to perforation.Etiologicfactors include:
❖ Autoimmune processes (collagenosis, marginal
keratitis, and scleroker-atitis).
❖
Trophic dysfunctions (pitting due to lack of tear film).
❖ Unknown degenerative processes (Terrien’s
marginal degeneration or Mooren’s ulcer).
These corneal changes are most frequently
observed in patients with rheuma-toid
arthritis. Treating the underlying disorder is essential in these
cases.Otherwise the changes are rare. Keratomalacia is a special form of the dis-order in which vitamin A deficiency causes xerosis of
the conjunctiva com-bined with night blindness. This disorder remains one of
the most frequent causes of blindness in the developing countries in which
malnutrition is prevalent.
Related Topics