Chapter: Ophthalmology: Cornea
Bacterial Keratitis
Bacterial Keratitis
Epidemiology: Over 90% of all corneal inflammations are caused by bacteria.
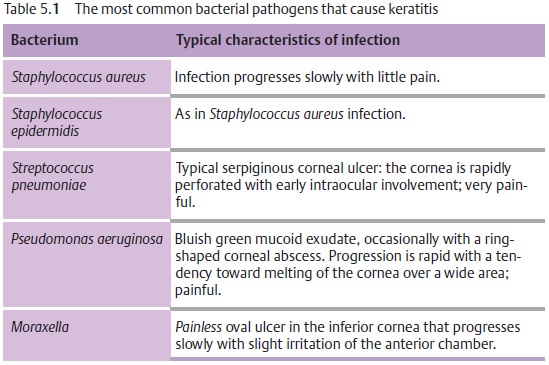
Etiology: The pathogens listed in Table 5.1are among the most frequentcauses of bacterial keratitis in the urban population in temperate climates.
Most bacteria are unable to penetrate the
cornea as long as the epi-thelium remains intact. Only gonococci and diphtheria
bacteria can penetrate an intact corneal epithelium.
Symptoms: Patients report moderate to severe pain (except inMoraxellainfections; see Table 5.1), photophobia, impaired vision,
tearing, and purulent discharge. Purulent
discharge is typical of bacterial
forms of keratitis; viral forms
produce a watery discharge.
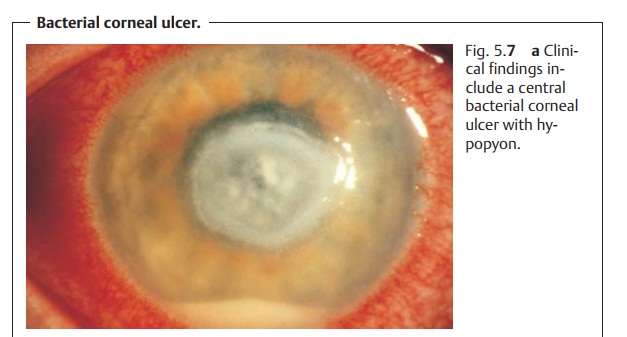
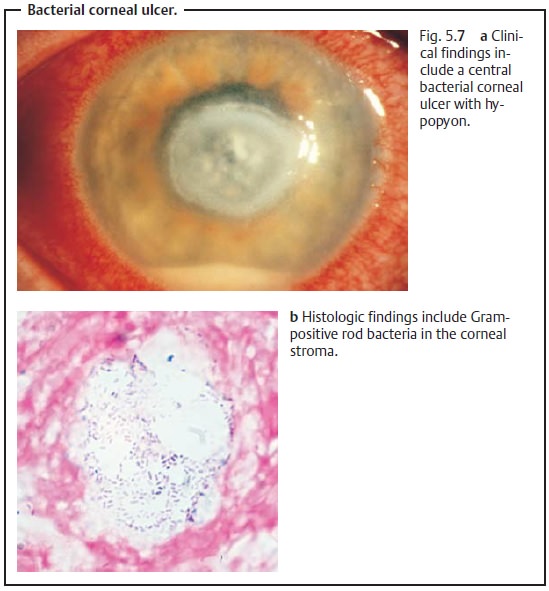
Diagnostic considerations: Positive identification of the pathogens is cru-cial. Serpiginous corneal ulcers are
frequently associated with severe reac-tion of the anterior chamber including
accumulation of cells and pus in the inferior anterior chamber (hypopyon, Fig.
5.7a) and posterior adhesions of the
iris and lens (posterior synechia).
Differential diagnosis: Fungi (positive identification of the pathogen isrequired to
exclude a fungus infection).
Treatment:
Because of the risk of perforation, any type
of corneal ulcer is an emer-gency requiring treatment by an ophthalmologist.
Conservative therapy.Treatment is initiated withtopical
antibiotics(such asofloxacin and polymyxin) with a very broad spectrum of
activity against most Gram-positive and Gram-negative organisms until the
results of pathogen and resistance testing are known. Immobilization of the
ciliary body and iris by therapeutic mydriasis is indicated in the presence of intraocular irritation (manifested by
hypopyon). Bacterial keratitis can be treated initially on an outpatient basis
with eyedrops and ointments.
An advanced
ulcer, i.e., a protracted clinical course, suggests indolence and poor
compliance on the part of the patient. Hospitalization
is indicated in these cases. Subconjunctival application of antibiotics may be
required to increase the effectiveness of the treatment.
Surgical treatment.Emergency keratoplasty is indicated to treat a desceme-tocele or
a perforated corneal ulcer (see emergency keratoplasty, p. 152). Broad areas of
superficial necrosis may require a conjunctival flap to accel-erate healing.
Stenosis or blockage of the lower lacrimal system that may impair healing of
the ulcer should be surgically corrected.
As soon as the results of bacteriologic and
resistance testing are avail-able, the physician should verify that the
pathogens will respond to cur-rent therapy.
Failure of keratitis to respond to treatment may be due to one of the follow-ing causes, particularly if the pathogen
has not been positively identified.
The patient is not applying the antibiotic (poor compliance).
The pathogen is resistant to the antibiotic.
The keratitis is not caused by bacteria but by one of the
following patho-gens:
❖ Herpes simplex virus.
❖ Fungi.
❖ Acanthamoeba.
❖Rare specific pathogens such as Nocardia or mycobacteria.
Related Topics