Chapter: Case Study in Obstetrics and Gynaecology: General Gynaecology
Case Study Reports: Intermenstrual Bleeding
INTERMENSTRUAL BLEEDING
History
A 48-year-old woman presents with intermenstrual bleeding
for 2 months. Episodes of bleeding occur any time in the cycle. This is usually
fresh red blood
and much lighter
than a normal period.
It can last
for 1–6 days.
There is no associated pain.
She has no hot
flushes or night sweats. She is sexually
active and has not noticed
vaginal dryness.
She
has
three
children
and
has
used
the
progesterone only pill for contraception for 5 years.
Her last smear
test was 2 years ago and all smears have been normal.
She takes no medi-
cation and has no other
relevant medical history.
Examination
The abdomen is unremarkable. Speculum examination shows a
slightly atrophic-looking vagina and cervix but there are no apparent cervical lesions and there is no current bleeding.
On bimanual examination the uterus is non-tender and
of normal size,
axial and mobile. There are no adnexal masses.

Questions
·
What is the diagnosis and differential diagnosis?
·
How
would you further
investigate and manage this woman?
Answer
The diagnosis is of an endometrial polyp,
as shown by the hydrosonography image (Fig. 1.1). These
can occur in women of any age although they are more common in older
women and may be asymptomatic or cause irregular bleeding or discharge. The aetiology is uncertain and the vast majority are benign. In this specific
case all the differential diag- noses are effectively excluded
by the history and examination.
Management
Any woman should
be investigated if bleeding occurs between periods. In women over the age
of 40 years, serious pathology, in particular endometrial carcinoma, should be excluded.
The polyp needs to be removed for two reasons:
·
to eliminate the cause of the bleeding
·
to
obtain a histological report to ensure that it is not malignant.
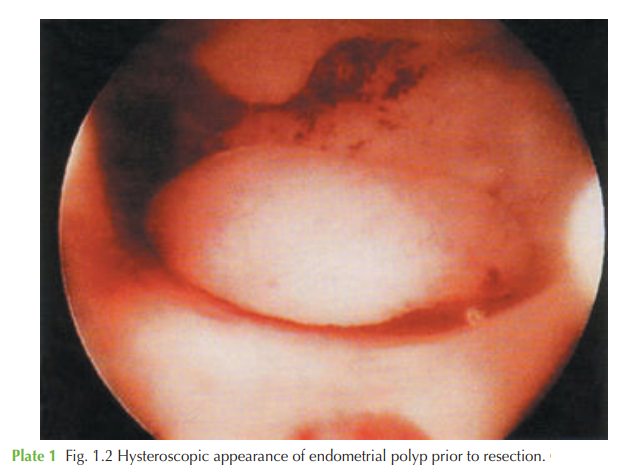
Management involves outpatient or day case hysteroscopy, and
resection of the polyp under direct vision using a diathermy
loop or other resection technique
(Fig. 1.2). This allows certainty that the polyp had been completely excised and also allows full inspec-
tion of the rest of the cavity
to check for
any other lesions
or suspicious areas.
In some settings, where
hysteroscopic facilities are not available, a dilatation and curettage may be
carried out with blind avulsion
of the polyp with polyp
forceps. This was the standard management in the past
but is not
the gold standard now, for
the reasons explained.
Related Topics