Chapter: Case Study in Obstetrics and Gynaecology: General Gynaecology
Case Study Reports: Anaemia
ANAEMIA
History
A
39-year-old woman is referred from the haematologist, with anaemia. She had been complaining of increasing tiredness and shortness of breath for
3 months, with
frequent headaches.
Her
periods occur every
24 days and
the first day
is generally moderate but the second
to fourth days are very heavy. She uses tampons and sanitary towels together. She has no pain.
Her last smear test was normal 2 years ago. She had no previous
gynaecological problems and takes no
medication.
Examination
The
woman is slim with pale conjunctivae. Abdominal, bimanual and speculum
examin- ation are unremarkable.
Questions
·
How do you interpret these findings?
·
What is the likely underlying diagnosis?
·
How would you manage this woman?
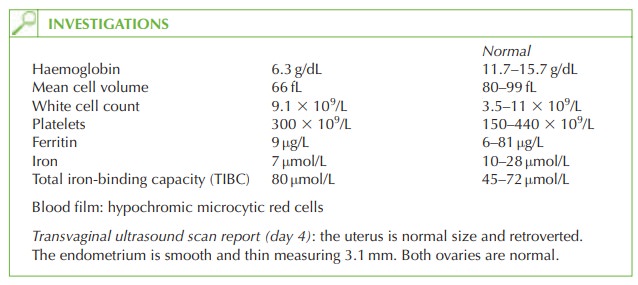
The blood count shows anaemia with
reduced mean cell corpuscular volume and low mean cell haemoglobin suggestive of a microcytic anaemia. Iron deficiency is the com- monest cause for this picture and is confirmed
by the low ferritin and iron, with raised
iron-binding capacity. The anaemia accounts for the breathlessness, tiredness
and headaches.
Menorrhagia is the commonest cause of anaemia
in women, and in this case is supported
by the history of excessive bleeding. The woman
herself may not recognize that her
periods are particularly heavy if she has always experienced heavy periods or if she thinks
it is normal for periods
to become heavier
as she gets older.
As
no other cause of heavy bleeding is apparent from the history
and the ultrasound is normal, then the underlying diagnosis is one of exclusion referred to as dysfunctional
uterine bleeding (DUB).
Management
The
anaemia should be treated with ferrous sulphate
200 mg twice daily until haemoglobin
and ferritin are normal. It may take 3–6
months for iron
stores to be fully replenished.
Tranexamic acid (an antifibrinolytic) should
be given during
menstruation to reduce
the amount of bleeding. It is contraindicated with a history
of thromboembolic disease.
The
levonorgestrel-releasing intrauterine device
is used for its action
on the endometrium to reduce menorrhagia, often causing amenorrhoea, though it is commonly associated with irregular bleeding for the first
3 months. The combined oral contraceptive pill is
effective for menorrhagia in young women (below 35 years).
If
these first-line management options are ineffective then endometrial ablation should be
considered, which destroys
the endometrium down to the basal layer.
It is successful in 80–85 per cent of women and they should
have completed their
family and use effective
contraception.
Hysterectomy is considered a ‘last
resort’ for DUB, due to the associated morbidity
Related Topics