Chapter: Case Study in Obstetrics and Gynaecology: General Gynaecology
Case Study Reports: Postmenopausal Bleeding
POSTMENOPAUSAL BLEEDING
History
A
58-year-old woman reports
postmenopausal bleeding for 6 months.
Initially she did not
pay much attention to it but she has had several episodes
and it now occurs most days. It is
generally light but for a few days recently it was almost
like a period. There is no asso- ciated pain. The woman has never married or been sexually
active. She has no previous gynaecological history
and has never
had a smear test. She was diagnosed with type 2 diabetes 4 years ago for which she takes oral hypoglycaemics. However she is not very compliant with diet modification, and her blood glucose is not well controlled such that
starting insulin is being considered.
Examination
The woman is obese with a body mass
index of 32 kg/m2.
Her blood pressure is 150/80 mmHg. The
abdomen is non-tender, but due to her adiposity it is not
possible to feel abdominal masses.
External genital examination is
unremarkable. Speculum and bimanual examination are not performed as she has
never been sexually active.
Transvaginal ultrasound was not
possible and a transabdominal ultrasound examination was therefore performed
with a full bladder.
Questions
·
What is the likely diagnosis?
·
If
this is confirmed how would you manage this patient?
ANSWER
Postmenopausal bleeding
should be considered to be due to endometrial carcinoma until
proven otherwise. In many cases the diagnosis
turns out to be benign.
However, in this case
early suspicion is raised by the risk
factors for endometrial carcinoma:
type 2 diabetes
·
obesity
·
nulliparity.
There is also a long history
of significant bleeding suggesting a more
significant path- ology. In women who can tolerate
the examination, the diagnosis may be made by outpa- tient endometrial sampling. In this case
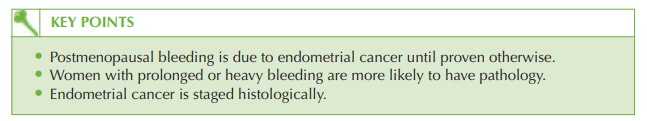
however, the inability to examine properly meant it was appropriate to investigate the uterine cavity and the rest of the lower genital tract under anaesthetic. The diagnosis of endometrial cancer
was confirmed on histology report from the curettage specimen.
Management
Management of endometrial carcinoma is simple total
abdominal hysterectomy and bilat-
eral salpingoophorectomy, as 90 per cent of women present with early-stage
disease. Magnetic resonance imaging
(MRI) scan prior
to the procedure may be carried out to
check for possible lymph node involvement, in which case lymph node biopsy should
be performed at the time of surgery. Cases
of stage 2 or greater
disease are less common and need adjuvant radiotherapy.
Histology is needed to stage
endometrial cancer:
·
stage 1: confined to the body of the uterus
·
1a limited to the endometrium
·
1b
invasion only of the inner
half of the myometrium
·
1c
invasion to the outer half the of the myometrium
·
stage 2: involving the uterus and cervix only
·
stage 3: extending beyond
the uterus but not beyond
the true pelvis
·
stage 4: extending beyond
the true pelvis
or into the
bladder or rectum.
The
woman should be advised that the prognosis is generally good with over 70 per cent survival at 5 years
for stage 1 disease, though
it is only 10 per cent
for stage 4 disease.
Related Topics