Chapter: Case Study in Obstetrics and Gynaecology: General Gynaecology
Case Study Reports: Postmenopausal Bleeding
POSTMENOPAUSAL BLEEDING
History
A
59-year-old woman awoke
with blood on her nightdress, which was bright
red but not heavy. There were no clots of blood and there was no associated pain. The bleeding
has recurred twice since
in similar amounts.
Her
last period was at the age of 49 years
and she has had no other intervening bleeding episodes. She suffered
hot flushes and night sweats
around the time of her menopause,
which have now stopped. She is sexually
active but has noticed vaginal
dryness on inter- course recently.
She
has always had normal cervical
smears, the last one being 7 months ago. She had
two children by spontaneous vaginal
delivery and had a laparoscopic sterilization aged
34 years. She has never
used hormone-replacement therapy
(HRT). She takes
atenolol for hypertension and
omeprazole for epigastric pain.
Examination
She
is slightly overweight. Abdominal examination is normal. The vulva and vagina
appear thin and atrophic and the cervix
is normal. The uterus is small and anteverted and with no palpable adnexal masses.
An
outpatient endometrial biopsy
is taken at the time
of examination and
sent for histo- logical examination.
Questions
·
What is the likely diagnosis?
·
How would you manage this patient?
Answer
Postmenopausal bleeding
is considered to be caused
by endometrial cancer
until proven otherwise. However,
only 10 per cent of women
with postmenopausal bleeding
are diagnosed with
endometrial cancer.
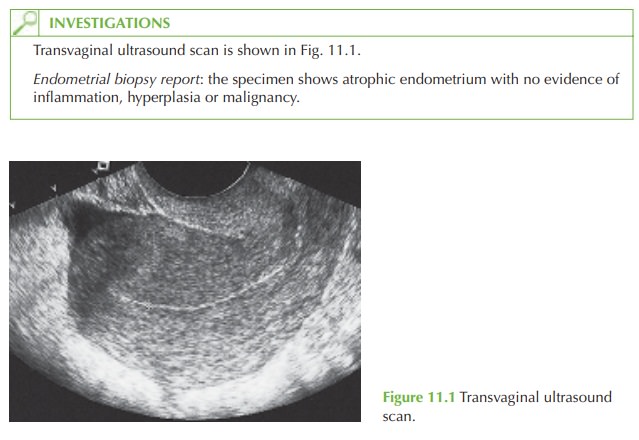
In this case the endometrium is <5 mm on ultrasound, which effectively excludes an endome-
trial malignancy or polyp. The normal endometrial biopsy report confirms the absence of endometrial
pathology. The smear history is
normal, and the cervix appears normal, excluding cervical
cancer. She is not taking any medication that may predispose to abnor- mal
bleeding.
The
diagnosis of atrophic
vaginitis can therefore be made by exclusion of serious causes, and is backed up by the
history of vaginal
dryness at sexual
intercourse and the
atrophic vulva and vagina noted on examination.
Management
Treatment is hormonal with a course
of topical oestrogen given daily for 3 weeks
and then twice weekly
for maintenance, for an initial
period of 2-3 months. An alternative solution is to give a combined form of systemic
HRT to protect the endometrium.
Some women are reluctant to use HRT
because of the associated risks, and therefore advice should be given about vaginal
lubricants which decrease
discomfort but have no
reparative value. If bleeding recurs
after treatment or the diagnosis is in doubt,
then fur- ther investigation with hysteroscopy and dilatation and curettage is needed.
Related Topics