Chapter: Case Study in Obstetrics and Gynaecology: General Gynaecology
Case Study Reports: Infertility
INFERTILITY
History
A
29-year-old woman and her partner
are seen in the gynaecology outpatient clinic with primary infertility. They stopped
using condoms 2 years ago
and have had
regular inter- course since
then. The partner
has no previous medical history of note. He drinks approxi- mately 8 units of alcohol per
week and does
not smoke. He works as a manager
in a hotel.
The
woman also has no specific
previous medical history
except for an appendectomy
aged 12 years. Her periods
occur every 31 to 46 days
and can be heavy at times but
not painful. There is no intermenstrual or postcoital bleeding. She has always
had normal smears and
has never had
any sexually transmitted infections. She takes
no medications, drinks approximately 6 units of alcohol per week and does not smoke.
Examination
On
examination her body mass index
(BMI) is 29 kg/m2. She has slight
acne on her face
and her chest.
There are no abdominal scars and the abdomen is non-tender with no masses
palpable. Speculum and bimanual
examination are normal. 3: AMENORRHOEA
Questions
·
What is the diagnosis?
·
How
would you further
investigate and manage this woman?
ANSWER
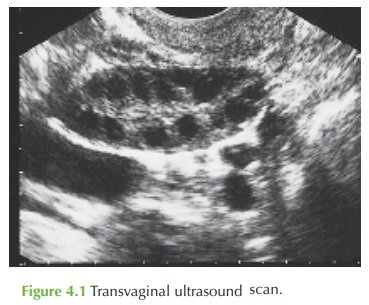
The diagnosis is of anovulatory
infertility due to polycystic ovarian syndrome
(PCOS). Anovulation is shown
by the progesterone level below 30 nmol/L, and
PCOS is suggested by several features including increased BMI, acne,
oligomenorrhoea, polycystic ovaries
on transvaginal ultrasound examination, increased androgen levels
and increased LH.
‘Polycystic ovaries’ (a
morphological description of enlarged ovaries with an increased number of follicles and dense stroma)
is present in up to 25 per cent of normal women. The diagnosis of PCOS is made on any combination of characteristic clinical, biochemical and ultrasound features.
PCOS is one of the commonest causes of infertility. However, up to 30 per cent of sub-
fertile couples have a multifactorial cause for their
problem. Hence complete
investigation of both partners
is essential prior
to treating the PCOS. This includes:
·
semen analysis
·
tubal patency test (hysterosalpingogram is usually sufficient)
·
laparoscopy and dye test
if pelvic inflammatory disease, adhesions or endometriosis
are suggested from the history.
Testing for rubella is also necessary, as is a recommendation to take folic
acid if this is not already taken. Other general
advice includes minimizing alcohol intake, avoiding smok- ing and ensuring regular intercourse (preferably 2–3 times per
week). The woman
should aim to reduce
weight as this commonly induces
ovulation in high-BMI
women with PCOS.
Treatment of anovulation
Clomifene citrate is the main
treatment to induce ovulation. The woman should be given 50 mg to take on day
2–6 of the menstrual cycle, with day 21 progesterone checked to confirm
ovulation. If ovulation occurs, then the clomifene is continued for up to six
cycles unless pregnancy occurs. If ovulation is not confirmed then the dose is
increased to 100 mg.
It is not recommended to take
clomifene for more than 6 months, due to a theoretical increased risk of
ovarian carcinoma. If clomifene fails, then further ovulation induction agents
and IVF need to be considered.
Related Topics