Chapter: Psychology: The Brain and the Nervous System
The Results of Cortical Damage
The Results of
Cortical Damage
We mentioned earlier that our
understanding of any brain region depends on multiple sources of data. For
studies of the association cortex, however, neuropsychological studies (studies
of brain damage) have often been our earliest indicators of a brain region’s
function. Let’s therefore take a closer look at the association cortex through
the lens provided by brain damage.
DISORDERS OF ACTION
Lesions in the cortex of the
frontal lobe sometimes produce apraxias—serious
distur-bances in the initiation or organization of voluntary action. In some
apraxias, the patient cannot perform well-known actions such as saluting or
waving good-bye when asked to do so. In other cases, seemingly simple actions
become fragmented and dis-organized. When asked to light a cigarette, the
patient may strike a match against a matchbox and then keep striking it after
it’s already burning; or, he may light the match and then put it into his mouth
instead of the cigarette. These deficits are not the result of simple
paralysis, since the patient can readily perform each part of the action by
itself. His problem is in initiating the sequence or in selecting the right
com-ponents and fitting them together.
Some apraxias may represent a
disconnection between the primary and nonprimary motor areas. The primary motor
area is responsible for producing the movements of individual muscles, but the
nonprimary motor areas must first organize and initiate the sequence. Indeed,
evidence suggests that the neurons in the nonprimary areas fire almost a full
second before the actual movement occurs; this confirms the role of these areas
in preparing the action (Deecke, Scheid, & Kornhuber, 1968). In short, the
non-primary areas seem to be responsible for “Get ready!” and “Get set!” Then,
at the “Go!” signal, the primary motor area takes over (Bear, Connors, &
Paradiso, 1996; Roland, Larsen, Lassen, & Skinhøj, 1980).
DISORDERS OF PERCEPTION AND ATTENTION
In other disorders, the patient
suffers a disruption in the way she perceives the world. Some patients (for
example) lose the ability to perceive motion, and so they cannot tell the speed
or direction of a moving object. As one patient put it, “When I’m looking at
the car first, it seems far away. But then when I want to cross the road,
suddenly the car is very near” (Zihl, Von Cramon, & Mai, 1983). Other
patients suffer brain damage that disrupts their ability to perceive color;
they describe the world as clothed only in “dirty shades of gray” (Gazzaniga,
Ivry, & Mangun, 2009).
Other patients seem able to see,
but they can’t recognize what they see. This pattern is referred to as visual agnosia and is usually produced
by damage to the occipital cor-tex or the rearmost part of the parietal cortex.
A patient with agnosia can often describe the shape, color, and texture of an
object before her eyes; but can recognize the object only through means other
than vision. For example, a patient shown an ordinary fork might describe it as
“points on top of a stick,” but she would not be able to name the object or
describe how to use it. However, the moment the patient feels the fork in her
hands, she easily identifies it.
Agnosia is a problem in recognition,
not in seeing. This is made
especially clear by a case in which a patient was shown a glove and asked what
it was. The patient described the glove as “a continuous surface infolded in
itself . . . [with] five outpouch-ings, if this is the word”. Perhaps, the
patient thought, it might be a “change purse . . . for coins of five sizes.”
Plainly, there’s nothing wrong with this per-son’s vision (or his verbal
fluency!), but it’s clear that he had no clue about what the glove actually
was.
One subtype of agnosia, known as prosopagnosia, usually involves damage
to areas in both the temporal and parietal lobes. Patients with prosopagnosia
have trouble recog-nizing faces—even immensely familiar faces. In one
often-quoted case, a person suffer-ing from prosopagnosia complained to a
waiter that another patron in the restaurant was rudely staring at him while he
ate. It turned out, however, that this prosopagnosic diner was looking into a mirror on the restaurant wall and had
failed to recognize his own reflection.
In some cases, the difficulties
associated with prosopagnosia can spread beyond faces: A farmer who developed
prosopagnosia lost the ability to tell his individual cows apart; a
prosopagnosic bird-watcher lost the ability to distinguish different types of warblers
(de Renzi, 2000; Farah & Feinberg, 2000). In one remarkable case, a
prosopagnosic patient lost the ability to tell cars apart; she could locate her
own car in a lot only by reading all the license plates until she found her own
(A. Damasio, H. Damasio, & Van Hoesen, 1982).
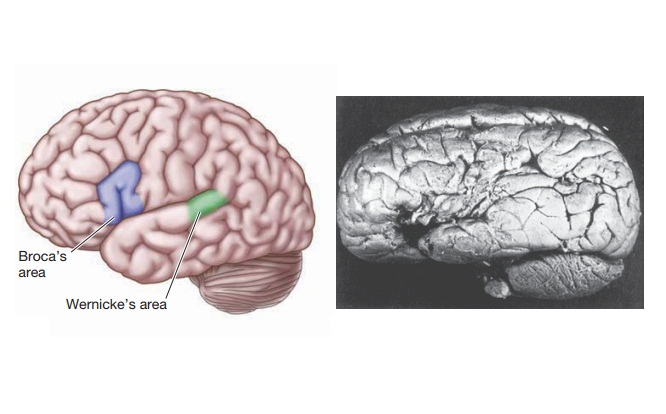
In still other disorders, the
patient’s problem is one of attention, so that the patient seems utterly
oblivious to certain aspects of the world. A striking example is the so-called neglect syndrome, which typically
results from damage to certain areas on the right side of the parietal lobe. A
patient with this disorder seems not to realize that the left-hand side of the
world exists. If asked, for example, to read compound words like toothpick or baseball, the patient reads pick
and ball. When asked to draw the face
of a clock, he squeezes all the numbers onto the clock’s right side (Figure
3.35). When eating , he selects and eats food only from the right side of his
plate. When dressing , he ignores the left shirt sleeve and pants leg; when
shav-ing , he leaves the left side of his face unshaven (Awh, Dhaliwal,
Christensen, & Matsukura, 2001; Duncan et al., 1999; Rafal & Robertson,
1995; Robertson & Manly, 1999).
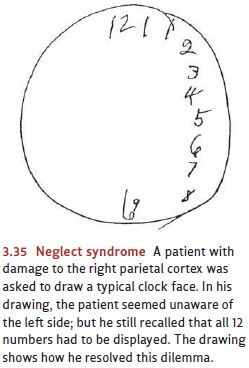
DISORDERS OF LANGUAGE
Other lesions in the cortex lead
to disruptions of the production or comprehension of language. Disorders of
this kind are called aphasias, and
they’re almost always pro-duced by lesions (strokes, typically) in the left
hemisphere.
Early studies suggested that
aphasias could be divided into two broad types: one that seemed primarily to
involve the production of speech, and one that seemed primarily to involve the
comprehension of speech. Aphasias of speech production
were often referred to as nonfluent
aphasias and typically involved lesions in a region of the left frontal
lobe, called Broca’s area after the
French physician Pierre-Paul Broca, who in 1861 first pre-dicted its relation
to speech (Figure 3.36). The result of this disorder may be mute silence, or
speech that resembles a staccato, spoken telegram: “Here . . . head . . .
opera-tion . . . here . . . speech . . . none . . . talking . . . what . . .
illness”.
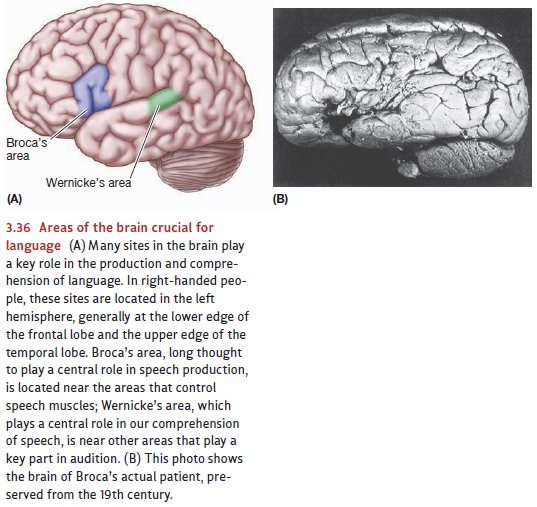
A different pattern is associated
with the so-called fluent aphasias—cases
in which patients seem able to produce speech but don’t understand what is said
to them, though they usually answer anyway. Unlike patients with nonfluent
aphasias, those with fluent aphasias talk freely and rapidly; but while they
utter many words, they say very little. The sentences they produce are
reasonably grammatical, but they’re “word salad”—largely composed of the little
filler words that provide scant information. A typical example is, “I was over
the other one, and then after they had been in the depart-ment, I was in this
one”. Fluent aphasias are usually asso-ciated with damage to a brain site known
as Wernicke’s area—a region that
borders on the auditory primary projection area and is named after the
nineteenth-century neurol-ogist Carl Wernicke.
This distinction—between
disorders of speech production associated with damage to Broca’s area and those
of comprehension associated with damage to Wernicke’s area—works as a coarse
characterization of aphasia. But to capture the real nature and the full range
of types of aphasia, we must considerably refine the distinction. The rea-son
is simple: Like most mental activities, speech production and comprehension
involve the coordination of many different steps, and many different processes.
These include processes needed to “look up” word meanings in one’s “mental
dictionary,” processes needed to figure out the structural relationships within
a sentence, processes needed to integrate information gleaned about a
sentence’s structure with the mean-ings of the words within the sentence, and
so on . Since each of these processes relies on its own set of brain pathways,
damage to those pathways disrupts the process. As a result, the disruption
observed in aphasia is often quite specific—it involves impairment to a
particular processing step, which then leads to disruption of all subsequent
processes that depend on that step. In many cases, this disruption seems mostly
to affect speech production; in other cases, the disruption is primarily
visible in comprehension; and in still other cases, the disruption is clear in
both activities (see Cabeza & Nyberg, 2000; Demonet, Wise, &
Frackowiak, 1993; Grodzinsky & Santi, 2008; Habib, Demonet, &
Frackowiak, 1996).
DISORDERS OF PLANNING AND SOCIALCOGNITION
Earlier, we referred to the
famous case of Phineas Gage. After an iron rod was driven through his head,
Gage could still speak and move fairly normally. But something subtler had
changed. A medical report on Gage put it this way:
He is fitful, irreverent,
indulging at times in the grossest profanity (which was not pre-viously his
custom), manifesting but little deference for his fellows, impatient of
restraint or advice when it conflicts with his desires, at times pertinaciously
obstinate, yet capricious and vacillating, devising many plans of future
operation, which are no sooner arranged than they are abandoned in turn for
others appearing more feasible. Previous to his injury . . . he possessed a
well-balanced mind . . . was energetic and per-sistent in executing all his
plans of operation. In this regard his mind was radically changed, so decidedly
that his friends and acquaintances said he was “no longer Gage.”
Gage’s symptoms fit reasonably
well with other things we know about the effect of damage to the frontmost part
of the frontal lobe—the prefrontal area
(Bradshaw, 2001; Lichter & Cummings, 2001; Milner & Petrides, 1984). In
general, damage here seems to disrupt the person’s executive control over her own thinking—and so she loses the
capacity to set pri-orities, override habits, make plans, choose a strategy,
ignore a distractor, and more.
This disruption shows up in many
aspects of the person’s behavior. Outside the lab-oratory, she is unable to
control her own impulses. She is likely to give in to habit and seize on
whatever temptation a situation offers. In the lab, we can document this
dis-ruption with the Wisconsin
Card-Sorting Task. In this task, the person is given a deck of cards, with
symbols on each card; the cards vary in the number, shape, and color of the
symbols. Initially, the person has to sort the cards according to (say) the
color of the symbols; midway through the task, however, the rule is changed.
Now he has to sort according to the symbols’ shape. Patients with frontal lobe
damage have enormous difficulty with the task and typically show a pattern of perseveration—continuing to sort
according to the initial rule despite explicit feedback that they’re now doing
the task incorrectly (e.g., Goldman-Rakic, 1998).
A related pattern is revealed
when patients with frontal lobe damage are asked to make a copy of a drawing.
For example, when asked to copy Figure 3.37A, a patient
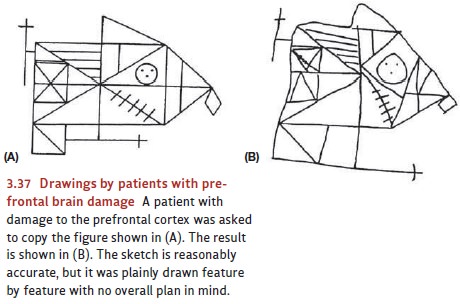
produced the drawing shown in
Figure 3.37B. The copy preserves many features of the original, but close
inspection makes it clear that the patient drew the copy with no particular
plan in mind. The large rectangle that defines much of the shape was never
drawn; the diagonal lines that organize the figure were drawn in a piecemeal
fashion. Many details are correctly reproduced but were not drawn in any sort
of order; instead, these details were added whenever they happened to catch the
patient’s attention (Kimberg, D’Esposito, & Farah, 1998; for more on the
brain’s processes of executive control, see Duncan, 1995; Gilbert &
Shallice, 2002; Kane & Engle, 2003; Stuss & Levine, 2002).
Related Topics