Chapter: Psychology: The Brain and the Nervous System
Plasticity: Repairing Damage to the Nervous System
Repairing
Damage to the Nervous System
Notice, then, that plasticity has
its advantages and disadvantages. On the positive side, plasticity makes it
possible to “rewire” the nervous system in response to new informa-tion and new
experience. On the negative side, plasticity may in some circumstances
undermine the stability of a pattern of neural connections and thus may be
disruptive. So perhaps it’s not surprising that different species have evolved
to have different degrees of plasticity, with the pattern presumably dependent
on that species’ need for flexibility or for longer-term retention.
There’s one arena, though, in
which plasticity is certainly desirable: If the nervous system is damaged
through injury or disease, the effects can be disastrous. It would be
wonderful, therefore, if the nervous system could repair itself by growing new
neurons or reestablishing new connections. This sort of self-repair is often
possible in the peripheral nervous system; there, neurons can regenerate their
axons even after the original axon has been severed. Unfortunately, this sort
of regrowth after damage seems not to occur in humans’ central nervous system,
and here, once nerve fibers are dam-aged, they generally stay damaged. (For
some of the mechanisms blocking this self-repair, see W.-Y.Kim & Snider,
2008.)
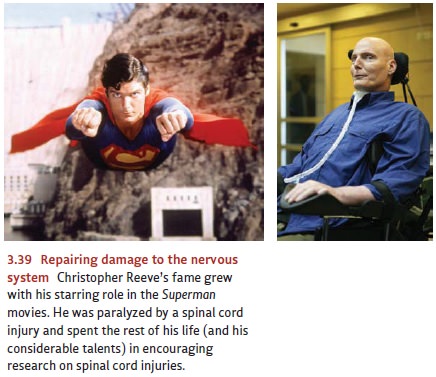
Is there some way, however, to
use the processes of plasticity observed in healthy brains to restore damaged
brains? If so, we might be able to repair the damage created by injury—such as
the spinal injury suf-fered by actor Christopher Reeve, well known for his role
in the Superman movies (Figure 3.39).
After his injury, Reeve spent the rest of his life paralyzed but devoted his
energy and talent to encouraging research on spinal cord injuries and other
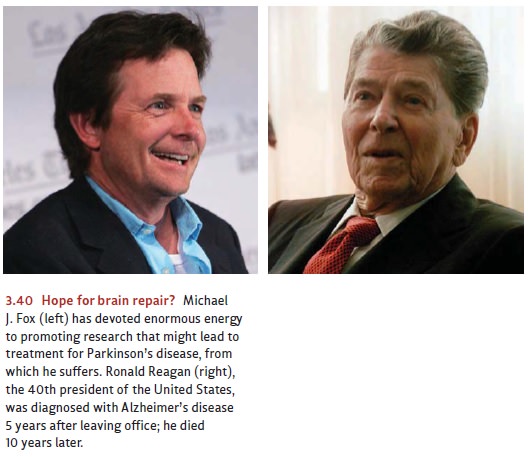
nerve damage. A means of restoring damaged brains might also give hope to those
suffering from Alzheimer’s dis-ease or Parkinson’s disease, both of which
involve the destruc-tion of brain tissue (Figure 3.40).
Researchers are actively
exploring these issues; some of their efforts are focused on encouraging the
growth of new neurons (e.g., W.-Y. Kim & Snider, 2008), and other research
is seeking to implant new tissue
into the brain in order to replace the damaged cells. Some of the most exciting
work, however, is in a third category and involves a mix of implanting tissue
and encouraging growth. Specifically, this effort involves implanting, into an
area of damage, the same sorts of stem
cells that are responsible for building the nervous system in the first
place. Stem cells are, in general, cells that are found in early stages of an
organ-ism’s development and that have not yet begun to specialize or
differentiate in any way. The idea in using these cells is that we would not be
replacing the damaged brain tissue directly. Instead, the stem cells would,
once in place, serve as precursors of the cells the brain needs—so the brain
could, in effect, grow its own replacements.
Preliminary studies in animals
suggest that when stem cells are injected into a patch of neurons, the cells
are—as we would hope—induced to turn into healthy neurons just like their
neighbors, taking the same shape, producing the same neurotransmitters, and
filling in for dead neurons (Holm et al., 2001; Isacson, 1999; Philips et al.,
2001; Sawamoto et al., 2001). Thus it seems plausible that stem-cell therapy may
provide a means of treatment for various forms of brain injury—and so far the
results have been quite encouraging (Kondziolka et al., 2000; Veizovic, Beech,
Stroemer, Watson, & Hodges, 2001). In one remarkable study, researchers
inserted human stem cells into the damaged spines of laboratory rats. The rats,
which had been paralyzed at the study’s start, recovered well enough so that
they could walk again (Cizkova et al., 2007).
Research in this domain
continues. In early 2009, the U.S. Food and Drug Administration gave permission
for the first clinical trials for stem-cell therapy in humans who had suffered
spinal cord injury. However, the progress of research in this arena has been
slow—largely due to an ethical debate over where the stem cells usually come
from. As part of a fertility treatment, a woman’s ova are sometimes removed,
fertilized in a labo-ratory, and allowed to develop into large masses of cells.
One of these masses is then placed back into the woman in hopes that it will
implant in the uterus and develop into a normal pregnancy. The other masses—the
ones not implanted—were for many years the main sources for stem cells, and
there lies the problem: In principle, these other masses might also have been
implanted and might also have developed into a human fetus. On that basis, some
people have argued that use of these cells for any other purpose is
essen-tially a form of abortion and thus is unacceptable to anyone who opposes
abortion.
This issue led President George
W. Bush to limit the use of federal research money for studies relying on
embryonic stem cells. Early in 2009, President Barack Obama reversed that
policy—so we can now expect the pace of research to accelerate. Meanwhile,
investigators are also seeking to develop alternative sources of stem cells;
this may allow us to avoid the ethical debate altogether. One way or another,
stem cell research is certain to continue; and in light of the evidence so far,
this research holds enormous promise for treating—and perhaps reversing—a range
of profoundly dis-abling diseases as well as helping people who have suffered
tragic injuries.
Related Topics