Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Radiation Therapy - Female Reproductive System
Radiation Therapy
Radiation
is usually the treatment of choice for squamous cell car-cinoma of the cervix,
depending on the stage of the cancer. In uterine and ovarian cancers, however,
radiation is usually an ad-junct to surgery. When radiation is the definitive
treatment of cervical cancer, a combination of external pelvic irradiation and
internal (intracavitary) irradiation may be used. Only in the ear-liest
microinvasive carcinomas of the cervix is intracavitary irra-diation used
alone. High cure rates can be expected with cervical cancer limited to the
cervix. As the disease extends into the para-metrium, the cure rate decreases.
Once the disease extends to the pelvic side walls, however, perhaps only one
third of patients are cured, although many more benefit from the palliative
effects of radiation (ie, reduction in tumor bulk and control of infection,
pain, and bleeding).
SIDE EFFECTS OF RADIATION THERAPY
Radiation
side effects are cumulative and tend to appear when the total dose exceeds the
body’s natural capacity to repair the dam-age caused by radiation. Radiation
enteritis, resulting in diarrhea and abdominal cramping, and radiation
cystitis, manifested by urinary frequency, urgency, and dysuria, may occur.
These effects are manifestations of the normal tissues’ response to radiation
therapy. Occasionally, severe reactions require interrupting treat-ment until
normal tissue repair occurs. Fatigue is one of the most bothersome side effects
and is often not relieved by rest.
The
radiation oncologist and nurse must carefully inform the patient in advance
about possible side effects and implement management strategies if they occur.
Such measures include di-etary control (restricting the amount of fiber,
roughage, and lac-tose) and the use of antispasmodic medications. The purpose
of a low-residue diet is to prevent frequent bowel movements and to avoid
blockage resulting from possible constriction of the gastro-intestinal tract.
An oncology dietitian may be consulted.
Evaluating
the patient’s and family’s physical, emotional, and learning needs is part of
the nursing assessment before and during treatment. Information overload, along
with anxiety that impairs learning, must be anticipated.
Any
method of therapy requires adequate preparation, educa-tion, and emotional
support. The patient who has been adequately prepared, supported, and educated
before treatment through ex-pert nursing care will find it easier to cope with
the rigors and stress of cancer and its treatment.
METHODS OF RADIATION THERAPY
Several
approaches are used to deliver radiation to the female re-productive system:
external radiation, intraoperative radiation therapy (IORT), and internal
(intracavitary) irradiation or brachytherapy. The cervix and uterus lend
themselves naturally to internal irradiation because they can serve as a
receptacle for radioactive sources.
External Radiation Therapy
This method
of delivering radiation destroys cancerous cells at the skin surface or deeper
in the body. Other methods of deliv-ering radiation therapy are more commonly
used to treat cancer of the female reproductive system than this method.
Intraoperative Radiation Therapy
IORT
allows radiation to be applied directly to the affected area during surgery. An
electron beam is directed at the disease site. This direct-view irradiation may
be used when para-aortic nodes are involved or for unresectable (inoperable) or
partially re-sectable neoplasms. Benefits include accurate beam direction
(which precisely limits the radiation to the tumor) and the abil-ity during
treatment to block sensitive organs from radiation. IORT is usually combined
with external-beam irradiation pre-operatively or postoperatively.
Internal (Intracavitary) Irradiation
The
patient receives an anesthetic agent and is examined, after which specially
prepared applicators are inserted into the en-dometrial cavity and vagina.
These devices are not loaded with radioactive material until the patient
returns to her room. X-rays are obtained to verify the precise relationship of
the applicator to the normal pelvic anatomy and to the tumor. Only when this
step is completed does the radiation oncologist load the applicators with
predetermined amounts of radioactive material. This procedure, called
afterloading, allows for precise control of the radiation exposure received by
the patient, with minimal exposure of the physician, nurse, and other health care
personnel. A patient undergoing internal radiation treatment remains isolated
in a pri-vate room until the application is completed. Adjacent rooms may need
to be evacuated and a lead shield placed at the doorway to the patient’s room.
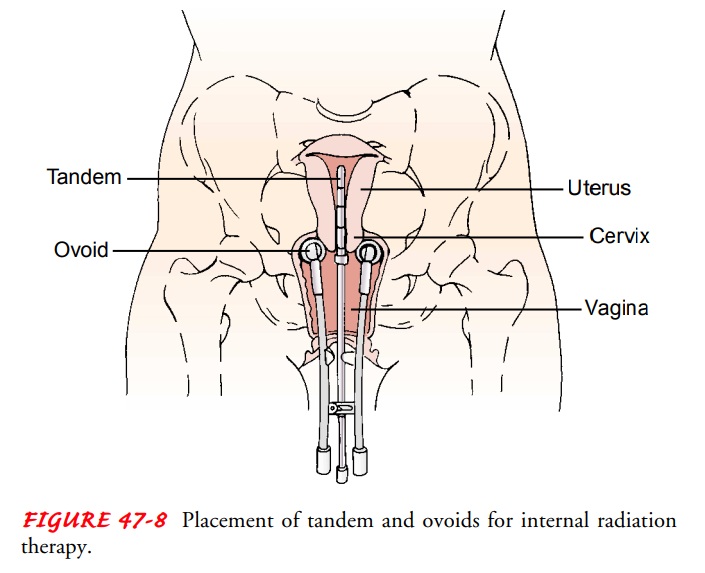
Of the
various applicators developed for intracavitary treat-ment, some are inserted
into the endometrial cavity and endocer-vical canal as multiple small
irradiators (eg, Heyman’s capsules). Others consist of a central tube (a tandem
or intrauterine “stem”)placed through the dilated endocervical canal into the
uterine cav-ity, which remains in a fixed relationship with the irradiators
placed in the upper vagina on each side of the cervix (vaginal ovoids) (Fig.
47-8).

When
the applicator is inserted, an indwelling urinary catheter is also inserted.
Vaginal packing is inserted to keep the applicator in place and to keep other
organs, such as the bladder and rec-tum, as far from the radioactive source as
possible. The objective of the internal treatment is to maintain the distribution
of inter-nal radiation at a fixed dosage throughout the application. Such
applications usually last 24 to 72 hours, depending on dose cal-culations made
by the radiation physicist.
Automated
high-dose-rate intracavitary brachytherapy sys-tems have been developed that
allow outpatient radiation therapy. Treatment time is shorter, thereby
decreasing patient discomfort. Staff exposure to radiation is also avoided.
Isotopes of radium and cesium are used for intracavitary irradiation.
NURSING CONSIDERATIONS FOR RADIATION SAFETY
Various
radioactive elements are used in intracavitary therapy. Regardless of the
specific agent used, diligent nursing care must be provided. The patient is
carefully observed and care is pro-vided; however, the nursing staff must
minimize radiation expo-sure to themselves as much as possible by applying the
principles of time, distance, and shielding, as follows:
· Minimize amount of time
near a radioactive source.
· Maximize distance from
radioactive source.
· Use required shielding
to minimize exposure.
Nurses
who are or may be pregnant should not be involved in the immediate care of such
patients. Nursing visits to the patient should be planned in advance to
minimize the amount of time the nurse is in contact with the patient. Additionally,
to minimize radiation exposure, the nurse remains as far away (ie, at the
en-trance to the room) from the radiation source as possible but makes special
efforts to provide some time to discuss the patient’s anxieties and fears.
The Radiation Safety Department will give specific safety pre-cautions to those who will be in contact with the patient, includ-ing health care providers and family. Nurses caring for the patient will receive directions about safe times and distances related to care provision to ensure that their occupational exposure is as low as reasonably achievable (ALARA). Other instructions vary but may include the following:
· Wear film badges or
pocket ion chambers to monitor exposure.
· Wear rubber gloves to
dispose of any soiled matter that may be contaminated. (These gloves, however,
do not provide protection from sealed radiation sources.)
· Provide specific laundry
and housekeeping directions.
· Keep the patient
restricted to her room and allow no visi-tors who are or may be pregnant or who
are younger than 18 years of age.
· Explain that a discharge
survey is usually performed by Ra-diation Safety Department personnel before
the patient leaves the room. The survey ensures that all sources of radi-ation
have been removed.
NURSING PRIORITIES FOR PATIENT CARE
Of the
many nursing concerns, primary concerns involve pro-viding the patient with
emotional support and physical comfort and not dislodging the applicator.
Although the radiation oncol-ogist takes steps to secure the internal
applicator in place and nursing personnel need not be preoccupied with the fear
that the applicator will be prematurely extruded, they should monitor to see
that the applicator or the radioactive sources have not been dislodged. Should
this happen, the nurse should avoid touching the radioactive object and notify
the Radiation Safety Department at once.
The
nurse needs to explain that during the treatment, the pa-tient must stay on
absolute bed rest. She may move from side to side with her back supported by a
pillow, and the head of the bed may be raised to 15 degrees. She should be
encouraged to prac-tice deep-breathing and coughing exercises and to flex and
extend the feet to stretch the calf muscles, promoting circulation and ve-nous
return. Elastic compression stockings are important. Back care, though
appreciated by the patient, needs to be performed within the minimal time
allowed at the bedside.
Usually
the patient receives a low-residue diet to prevent fre-quent bowel movements.
In addition, a urinary catheter will be in place and must be inspected
frequently to ensure that it drains properly. The chief hazard of improper
drainage is that the blad-der may become distended and its walls exposed to
radiation. Al-though perineal care is not performed at this time, any profuse
discharge should be reported immediately to the radiation on-cologist or
gynecologic surgeon.
Additional
nursing interventions include observing the patient for temperature elevation,
nausea, and vomiting. These symptoms should be reported because they may
indicate such complications as infection or perforation.
Patient
teaching includes informing the patient that abdomi-nal fullness, cramping,
backache, and the urge to void are normal feelings during therapy. Severe pain
should not occur. Adminis-tering mild opioid agents, muscle relaxants, or
sedative medica-tions may be helpful.
APPLICATOR REMOVAL
The
radiation oncologist calculates precisely the radiation dose. At the end of the
prescribed period, the nurse may be requested to assist the physician in
removing the applicator. Because the sources are afterloaded, they can be
removed by the physician in the same manner as they were inserted. This does
not require local or general anesthesia and is performed in the patient’s room.
Medicating the patient with a mild sedative agent may be re-quired, however,
before the applicator is removed.
POST-TREATMENT CARE
Progressive
ambulation is recommended after any period of en-forced bed rest. Diet may be
offered as tolerated. The patient may shower as soon as she wishes but should
be instructed not to douche after removal of the applicator. Because the cervix
may have been dilated, any chance of bacterial contamination should be
minimized.
Both
before and after treatment, nurses caring for patients un-dergoing radiation
therapy need to assess any misconceptions about this mode of treatment that the
patient and family may have. The oncology clinical nurse specialist may be a
valuable re-source for information and problem solving, if necessary.
Related Topics