Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Pelvic Infection (Pelvic Inflammatory Disease)
PELVIC
INFECTION (PELVIC INFLAMMATORY DISEASE)
Pelvic inflammatory disease (PID) is an inflammatory
condi-tion of the pelvic cavity that may begin with cervicitis and may involve
the uterus (endometritis), fallopian tubes (salpingitis), ovaries (oophoritis), pelvic peritoneum, or pelvic
vascular system. Infection, which may be acute, subacute, recurrent, or chronic
and localized or widespread, is usually caused by bacteria but may be
attributed to a virus, fungus, or parasite. Gonorrheal and chlamydial organisms
are the most likely causes. Cytomegalovirus (CMV) has also been implicated.
This condition can result in the fallopian tubes becoming narrowed and scarred,
which increases the risk for ectopic pregnancy (fertilized eggs become trapped
in the tube), infertility, recurrent pelvic pain, tubo-ovarian abscess, and recurrent disease. Rupture
of a tubo-ovarian abscess has a 5% to 10% mortality rate and usually
necessitates a complete hys-terectomy. About 1 million women are diagnosed with
PID each year in the United States; most are younger than 25 years of age, and
one fourth of them have serious sequelae (ie, infertility, ec-topic pregnancy,
or chronic pelvic pain) (Rein, Kasler, Irwin & Rabiee, 2000). PID is the
most common gynecologic cause of hos-pital admissions in the United States. The
true incidence of PID is unknown because most cases are asymptomatic (Ross,
2001).
Pathophysiology
The
exact pathogenesis of PID has not been determined, but it is presumed that
organisms usually enter the body through the vagina, pass through the cervical
canal, colonize the endocervix, and move upward into the uterus. Under various
conditions, the organisms may proceed to one or both fallopian tubes and
ovaries and into the pelvis. In bacterial infections that occur after
child-birth or abortion, pathogens are disseminated directly through the
tissues that support the uterus by way of the lymphatics and blood vessels
(Fig. 47-1). In pregnancy, the increased blood sup-ply required by the placenta
provides more pathways for infec-tion. These postpartum and postabortion
infections tend to be unilateral. Infections can cause perihepatic inflammation
when the organism invades the peritoneum.
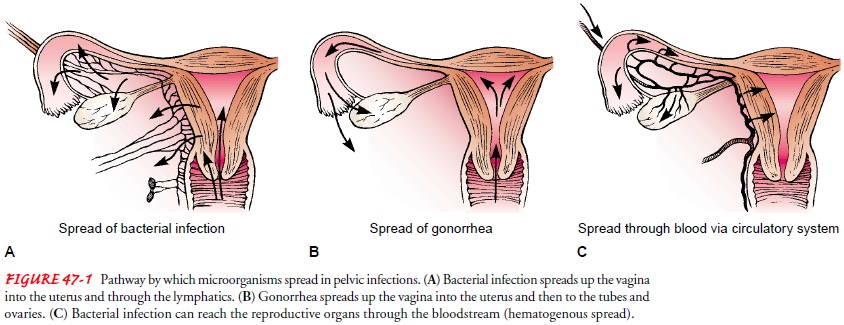
In
gonorrheal infections, the gonococci pass through the cer-vical canal and into
the uterus, where the environment, especially during menstruation, allows them
to multiply rapidly and spread to the fallopian tubes and into the pelvis (see
Fig. 47-1). The in-fection is usually bilateral. In rare instances, organisms (eg,
tu-berculosis) gain access to the reproductive organs by way of the bloodstream
from the lungs (see Fig. 47-1). One of the most common causes of salpingitis
(inflammation of the fallopian tube) is chlamydia, possibly accompanied by
gonorrhea.
Pelvic
infection is most commonly caused by sexual transmis-sion but can also occur
with invasive procedures such as endome-trial biopsy, surgical abortion,
hysteroscopy, or IUD insertion. Bacterial vaginosis, a vaginal infection, may
predispose women to pelvic infection. Risk factors include early age at first
intercourse, multiple sexual partners, frequent intercourse, intercourse
with-out condoms, sex with a partner with an STD, and a history of STDs or
previous pelvic infection.
Clinical Manifestations
Symptoms
of pelvic infection usually begin with vaginal dis-charge, dyspareunia, lower
abdominal pelvic pain, and tenderness that occurs after menses. Pain may
increase while voiding or with defecation. Other symptoms include fever,
general malaise, anorexia, nausea, headache, and possibly vomiting. On pelvic
ex-amination, intense tenderness may be noted on palpation of the uterus or
movement of the cervix (cervical motion tenderness). Symptoms may be acute and
severe or low-grade and subtle.
Complications
Pelvic
or generalized peritonitis, abscesses, strictures, and fallopian tube
obstruction may develop. Obstruction may cause an ectopic pregnancy in the
future if a fertilized egg cannot pass a tubal stric-ture, or scar tissue may
occlude the tubes, resulting in sterility. Ad-hesions are common and often
result in chronic pelvic pain; they eventually may require removal of the
uterus, fallopian tubes, and ovaries. Other complications include bacteremia
with septic shock and thrombophlebitis with possible embolization.
Medical Management
Broad-spectrum antibiotic therapy is prescribed. Women with mild infections may be treated as outpatients (Ness, Soper, Holley et al., 2002c), but hospitalization may be necessary. Intensive therapy includes bed rest, intravenous fluids, and intravenous antibiotic therapy.
If the patient has abdominal distention or ileus, naso-gastric intubation and
suction are initiated. Carefully monitor-ing vital signs and symptoms assists
in evaluating the status of the infection. Treating sexual partners is
necessary to prevent re-infection.
Nursing Management
Infection
takes a toll, both physically and emotionally. The pa-tient may feel well one
day and experience vague symptoms and discomfort the next. She may also suffer
from constipation and menstrual difficulties.
The
hospitalized patient is maintained on bed rest and is usu-ally placed in the
semi-Fowler’s position to facilitate dependent drainage. Accurate recording of
vital signs and the characteristics and amount of vaginal discharge is
necessary as a guide to therapy.
The
nurse administers analgesic agents as prescribed for pain relief. Heat applied
safely to the abdomen may also provide some pain relief and comfort.
The
nurse minimizes the transmission of infection to others by carefully handling
perineal pads with gloves, discarding the soiled pad according to hospital
guidelines for disposal of biohazardous material, and performing meticulous
hand hygiene.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
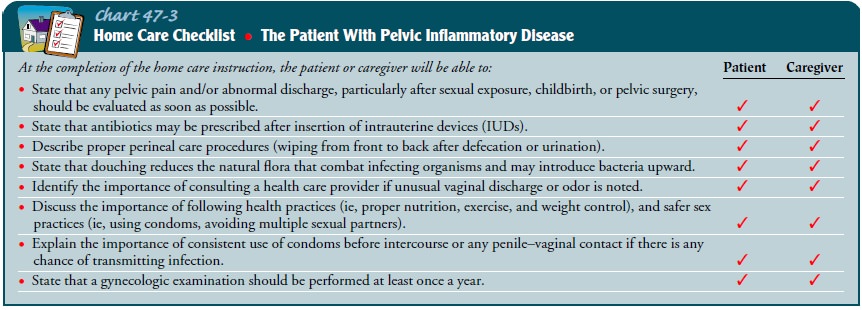
The patient
must be informed ofthe need for precautions and must be encouraged to take part
in procedures to prevent infecting others and protecting herself from
reinfection. If a partner is not well known or has had other sexual partners
recently, use of condoms may prevent life-threat-ening infection and its
sequelae. If reinfection occurs or if the in-fection spreads, symptoms may
include abdominal pain, nausea and vomiting, fever, malaise, malodorous
purulent vaginal dis-charge, and leukocytosis. Patient teaching consists of
explaining how pelvic infections occur, how they can be controlled and avoided,
and their signs and symptoms. Guidelines and instruc-tions provided to the
patient are summarized in the accompany-ing Home Care Checklist (Chart 47-3).
All
patients who have had PID need to be informed of the signs and symptoms of
ectopic pregnancy (pain, abnormal bleed-ing, delayed menses, faintness,
dizziness, and shoulder pain) be-cause they are prone to this complication.
Related Topics