Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Cancer of the Ovary
CANCER
OF THE OVARY
Ovarian
cancer causes more deaths than any other cancer of the female reproductive
system. About 75% of cases are detected at a late stage (Duffy, 2001). The
ovary is a common site of primary as well as metastatic lesions from other
cancers. Most cases affect women ages 50 to 59. The incidence of ovarian cancer
is highest in industrialized countries, except for Japan, where its incidence
is low.
A
woman with ovarian cancer has a threefold to fourfold in-creased risk for
breast cancer, and women with breast cancer have an increased risk for ovarian
cancer. No definitive causative fac-tors have been determined, but oral
contraceptives appear to pro-vide a protective effect. Heredity plays a part,
and many physicians advocate pelvic examinations every 6 months for women who
have one or two relatives with ovarian cancer. Despite careful ex-amination,
ovarian tumors are often difficult to detect because they are usually deep in
the pelvis. No early screening mechanism exists at present, although tumor
markers are being explored. Transvaginal ultrasound and Ca-125 antigen testing
are helpful in those at high risk for this condition. Tumor-associated antigens
are helpful in follow-up care after diagnosis and treatment but not in early
general screening.
Advances
in our knowledge of genetics are changing the ap-proaches to detecting and
treating breast and ovarian cancer. Some families have specific genes that
predispose them to various cancers. BRCA-1 is a genetic mutation that results
in an increased risk for breast and ovarian cancer. BRCA-2 is another genetic
mutation that may result in increased risk for both female and male breast
cancers and for ovarian cancer (Duffy, 2001). Other mutations are also under
study. Testing for susceptibility is in the early stages at centers that have
expertise in genetics, testing, and counseling. Testing is indicated when a
family history of three or more cases of closely related members includes
premenopausal breast cancer or ovarian cancer. One member with cancer is
tested, and if the results are positive, other members without can-cer may
undergo testing.
Much
more needs to be learned about the risks associated with some mutations, the
reliability of testing, and the efficacy of follow-up. Confidentiality and
insurance risks are ethical issues that need clarification. Because there are
no primary methods of preventing breast or ovarian cancer, emotional distress is
also a problem. Patients with concerns about their family history should be
referred to a cancer genetics center to obtain information and testing, if
indicated. Women with inherited types of ovarian can-cer tend to be younger
when the diagnosis is made than the aver-age age of 59 years at the time of
diagnosis.
Risk
factors also include nulliparity and infertility. Older age is a major risk
factor because the incidence of this disease peaks in the eighth decade of
life. High dietary fat intake, mumps be-fore menarche, use of talc in the
perineal area, and family history are suspected to increase risk, while
multiparity, oral contracep-tive use, breastfeeding, and anovulatory disorders
may be protec-tive. Survival rates depend on the stage of the cancer at
diagnosis.
Fifteen
percent of all new cases of ovarian tumors have low malignancy potential (LMP
tumors). These borderline tumors resemble ovarian cancer but have much more
favorable out-comes. Women diagnosed with this type of cancer tend to be
younger, in their early 40s. A conservative surgical approach is now used. The
affected ovary is removed, but the uterus and the contralateral ovary may
remain. Adjuvant therapy may not be warranted for these tumors.
Clinical Manifestations
Symptoms
are nonspecific and include increased abdominal girth, pelvic pressure,
bloating, indigestion, flatulence, increased waist size, leg pain, and pelvic
pain. Symptoms are often vague, and many women ignore the symptoms. Ovarian
cancer is often silent, but enlargement of the abdomen from an accumulation of
fluid is the most common sign. Any woman with gastrointestinal symptoms and
without a known diagnosis must be evaluated with ovarian cancer in mind.
Flatulence, fullness after a light meal, and increasing abdominal girth are
significant symptoms.
Vague,
undiagnosed, persistent gastrointestinal symptoms should alert the nurse to the
possibility of an early ovarian malig-nancy. A palpable ovary in a woman who
has gone through meno-pause is investigated because ovaries normally become
smaller and less palpable after menopause.
Assessment and Diagnostic Findings
Any
enlarged ovary must be investigated. Pelvic examination often does not detect
early ovarian cancer, and pelvic imaging tech-niques are not always definitive.
About 75% of ovarian cancers have metastasized by the time of diagnosis; about
60% have spread beyond the pelvis. Of the many different ovarian cancer cell
types, epithelial tumors constitute 90%. Germ cell tumors and stromal tumors
make up the other 10%.
Medical Management
SURGICAL MANAGEMENT
Surgical
staging, exploration, and reduction of tumor mass are the basics of treatment.
Surgical removal is the treatment of choice; the preoperative workup includes a
barium enema or colonoscopy, upper gastrointestinal series, chest x-rays, and
intravenous urog-raphy. CT scans and immunoscintigraphy, the use of radioactive
antibodies, may be used preoperatively to rule out intra-abdominal metastasis.
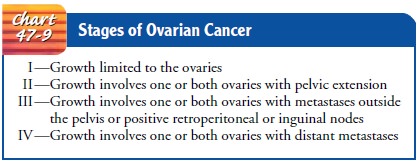
Staging the tumor is important to guide treatment (Chart 47-9). A total
abdominal hysterectomy with removal of the fallopian tubes and ovaries and the
omentum (bilateral salpingo-oophorectomy and omentectomy) is the standard
procedure for early disease.
PHARMACOLOGIC THERAPY
Chemotherapy
often follows surgery, usually with cyclo-phosphamide (Cytoxan), doxorubicin
(Adriamycin), cisplatin (Platinol-AQ), carboplatin (Paraplatin), or paclitaxel
(Taxol). Hexamethylmelamine (Hexalen), ifosfamide (Ifex), bone marrow
transplantation, and peripheral blood stem cell support may also be used.
Paclitaxel, cisplatin, and carboplatin are most often used because of their
excellent clinical benefits and manageable toxic-ity. Leukopenia,
neurotoxicity, and fever may occur.
Paclitaxel,
an agent derived from the Pacific yew tree, works by causing microtubules
within the cells to gather and prevents the breakdown of these threadlike
structures. In general, cells can-not function when they are clogged with
microtubules and can-not divide. Because this medication often causes
leukopenia, the patient may need to take granulocyte colony-stimulating factor
as well.
Paclitaxel
is contraindicated in patients with hypersensitivity to medications formulated
in polyoxyethylated castor oil and in patients with baseline neutropenia.
Because of possible adverse cardiac effects, paclitaxel is not used in patients
with cardiac dis-orders. Hypotension, dyspnea, angioedema, and urticaria
indi-cate severe reactions that usually occur soon after the first and second
doses are administered. The nurse must be prepared to as-sist in treating
anaphylaxis. The patient should be prepared for inevitable hair loss.
Cisplatin
is used frequently in chemotherapeutic treatment of ovarian cancer, both alone
and in combination with other agents, and in intraperitoneal applications.
Patients may require bone marrow transplantation or stem cell transplantation
to treat ovarian cancer. Intraperitoneal chemotherapy with cisplatin may
provide a prom-ising mode of treatment.
Carboplatin may be used in the initial treatment of advanced ovarian cancer in combination with other chemotherapeutic agents. It may also be used in patients with recurrence of ovarian cancer after other chemotherapy, including cisplatin. It must be used with caution in patients with renal impairment.
Other
medications include topotecan (Hycamtin), irinotecan (Camptosar), gemcitabine
(Gemzar), vinorelbine (Navelbine), li-posomal doxorubicin (Doxil), and
docetaxel (Taxotere). Differ-ent combinations, different regimens, different
routes, and use of growth factors are being investigated.
Liposomal therapy, delivery of chemotherapy in a
liposome,allows the highest possible dose of chemotherapy to the tumor tar-get
with a reduction in adverse effects. Liposomes are used as drug carriers because
they are nontoxic, biodegradable, easily available, and relatively inexpensive.
This encapsulated chemotherapy allows increased duration of action and better
targeting. The encapsula-tion of doxorubicin lessens the incidence of nausea,
vomiting, and alopecia. The patient must be monitored for bone marrow
sup-pression. Gastrointestinal and cardiac effects may also occur. These
medications are administered by oncology nurses as a slow intra-venous infusion
over 60 to 90 minutes.
Genetic
engineering and identification of cancer genes may make gene therapy a future
possibility. Gene therapy is under in-vestigation. Radiation may be helpful and
is more useful in some types of ovarian cancer than others.
After
adjunct therapies are completed, a second-look lapa-roscopy or a laparotomy may
be performed in some clinical cen-ters to evaluate the treatment results and to
obtain multiple tissue samples for biopsy. Occasionally, catheters are left in
place if radio-active agents are to be used postoperatively. Chemotherapy is
the most common form of treatment in advanced disease.
Nursing Management
Nursing
measures include those related to the patient’s treatment plan, be it surgery,
chemotherapy, radiation, or palliation. Emo-tional support, comfort measures,
and information, plus atten-tiveness and caring, are meaningful aids to the
patient and her family.
Nursing
interventions after pelvic surgery to remove the tumor are similar to those
after other abdominal surgeries. If ovarian cancer occurs in a young woman and
the tumor is uni-lateral, it is removed. Childbearing, if desired, is
encouraged in the near future. After childbirth, surgical re-exploration may be
performed and the remaining ovary may be removed. If both ovaries are involved,
surgery is performed and chemotherapy follows.
Patients
with advanced ovarian cancer may develop ascites and pleural effusion. Nursing
care may include administering intra-venous therapy to alleviate fluid and
electrolyte imbalances, initi-ating parenteral nutrition to provide adequate
nutrition, providing postoperative care after intestinal bypass to alleviate an
obstruction, and providing pain relief and managing drainage tubes. These
con-ditions are complex and often require assistance and support from an
oncology nurse specialist. Comfort measures for women with ascites may include
providing small frequent meals, decreasing fluid intake, administering diuretic
agents, and providing rest. Patients with pleural effusion may experience
shortness of breath, hypoxia, pleuritic chest pain, and cough. Thoracentesis is
usually performed.
Related Topics