Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Uterine Prolapse - Structural Disorders
UTERINE
PROLAPSE
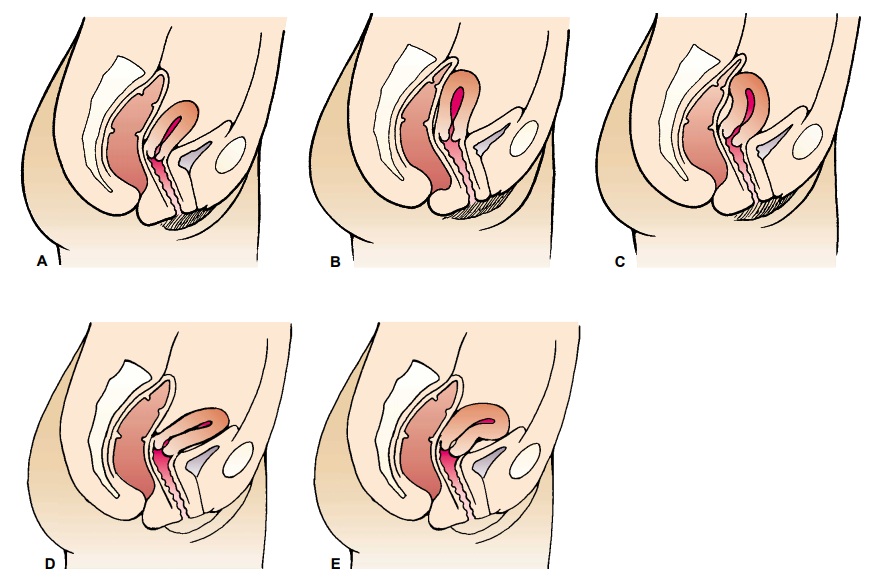
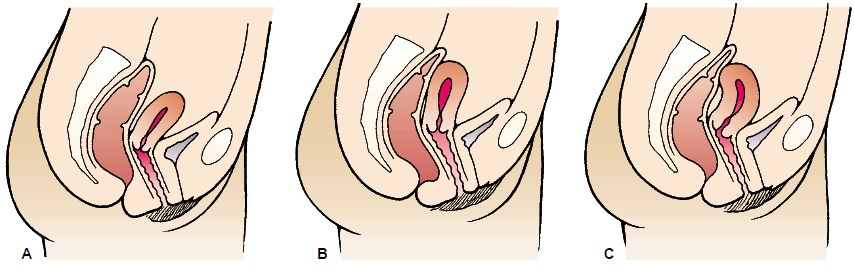
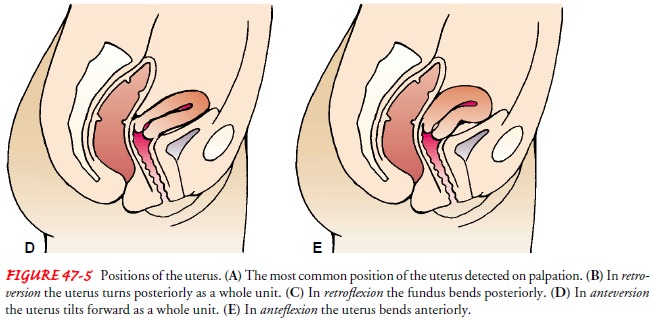
Usually,
the uterus and the cervix lie at right angles to the long axis of the vagina
and with the body of the uterus inclined slightly for-ward. The uterus is
normally freely movable upon examination. Individual variations may result in
an anterior, middle, or poste-rior uterine position. A backward positioning of
the uterus, known as retroversion and retroflexion, is not uncommon (Fig.
47-5).
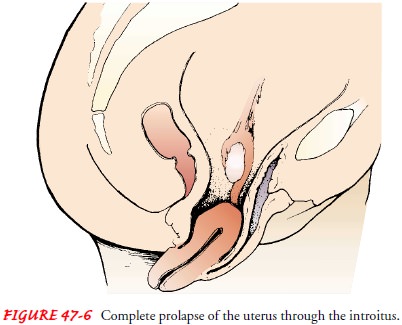
If the
structures that support the uterus weaken (typically from childbirth), the
uterus may work its way down the vaginal canal (prolapse) and even appear
outside the vaginal orifice (pro-cidentia) (Fig. 47-6). As the uterus descends,
it may pull the vagi-nal walls and even the bladder and rectum with it.
Symptoms include pressure and urinary problems (incontinence or reten-tion)
from displacement of the bladder. The problems are aggra-vated when the woman
coughs, lifts a heavy object, or stands for a long time. Normal activities,
even walking up stairs, may ag-gravate the problem.
Medical Management
Pessaries
and surgery are two options for treatment. If surgery is the method of
treatment used, the uterus is sutured back into place and repaired to
strengthen and tighten the muscle bands. In post-menopausal women, the uterus
may be removed (hysterectomy). For
elderly women or those who are too ill to withstand the strain of surgery,
pessaries may be the treatment of choice.
Nursing Management
IMPLEMENTING PREVENTIVE MEASURES
Some
problems related to “relaxed” pelvic muscles (cystocele, rec-tocele, and
uterine prolapse) may be prevented. During pregnancy, early visits to the
health care provider permit early detection of problems. During the postpartum
period, the woman can be taught to perform Kegel exercises to strengthen the
muscles that support the uterus.
Delays
in obtaining evaluation and treatment may result in complications such as
infection, cervical ulceration, cystitis, and hemorrhoids. The nurse encourages
the patient to obtain prompt treatment for these structural disorders.
IMPLEMENTING PREOPERATIVE NURSING CARE
Before
surgery, the patient needs to know the extent of the pro-posed surgery, the
expectations for the postoperative period, and the effect of surgery on future
sexual function. In addition, the pa-tient having a rectocele repair needs to
know that before surgery, a laxative and a cleansing enema may be prescribed.
She may be asked to administer these at home the day before surgery. A
per-ineal shave may be prescribed as well. The patient is usually placed in a
lithotomy position for surgery, with special attention given to moving both
legs in and out of the stirrups simultaneously to prevent muscle strain and
excess pressure on the legs and thighs.
INITIATING POSTOPERATIVE NURSING CARE
Immediate
postoperative goals include preventing infection and pressure on any existing
suture line. This may require perineal care and may preclude using dressings.
The patient is encouraged to void within a few hours after surgery for
cystocele and com-plete tear. If the patient does not void within this period
and re-ports discomfort or pain in the bladder region after 6 hours, she will
need to be catheterized. Some physicians prefer to leave an indwelling catheter
in place for 2 to 4 days, so some women may return home with a catheter in
place. After each voiding or bowel movement, the perineum is cleansed with
warm, sterile saline so-lution and dried with sterile absorbent material if a
perineal inci-sion has been made.
After
an external perineal repair, several methods are used in caring for the
sutures. In one method, the sutures are left alone until healing occurs (in 5
to 10 days). Thereafter, daily vaginal douches with sterile saline solution may
be administered during recovery. In another method—the wet method—small,
sterile saline douches are administered twice daily, beginning on the day after
surgery and continuing throughout recovery. A heat lamp or hair dryer may be
used to help dry the area and promote heal-ing. Commercially available sprays
containing combined anti-septic and anesthetic solutions are soothing and
effective, and an ice pack applied locally may relieve discomfort. However, the
weight of the ice bag must rest on the bed and not on the patient.
Routine
postoperative care is similar to that given after ab-dominal surgery. The
patient is positioned in bed with the head and knees elevated slightly. The
patient may go home the day of or the day after surgery; the duration of the
hospital stay depends on the surgical approach used.
After
surgery for a complete perineal laceration (through the rectal sphincter),
special care and attention are required. The blad-der is drained through the
catheter to prevent strain on the sutures. Throughout recovery, stool-softening
agents are administered nightly after the patient begins a soft diet.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Predischarge
instructions includeinformation pertaining to the gynecologist’s postoperative
in-structions related to douching, using mild laxatives, performing exercise as
recommended, and avoiding lifting heavy objects or standing for prolonged
periods. The patient is reminded to re-turn to the gynecologist for a follow-up
visit and to consult with the physician about when it is safe to resume sexual
intercourse.
The
patient is instructed to report any pelvic pain, unusual discharge, inability
to carry out personal hygiene, and vaginal bleeding. She is advised to continue
with perineal exercises, which are recommended to improve muscle strength and
tone.
Related Topics