Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Cancer of the Cervix
CANCER
OF THE CERVIX
Carcinoma
of the cervix is predominantly squamous cell cancer (10% are adenocarcinomas).
During the past 20 years, the inci-dence of invasive cervical cancer has
decreased from 14.2 cases per 100,000 women to 7.8 cases per 100,000 women. It
is less com-mon than it once was because of early detection of cell changes by
Pap smear. However, it is still the third most common female reproductive
cancer and affects about 13,000 women in the United States every year (American
Cancer Society, 2002). Cervical cancer occurs most commonly in women ages 30 to
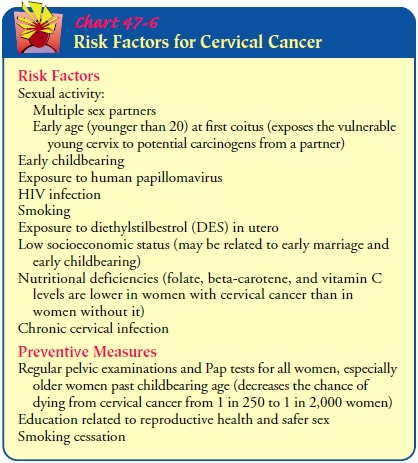
45, but it can occur as early as age 18. Risk factors include multiple sex
partners, early age at first coitus, short interval between menarche and first
coitus, sexual contact with men whose partners have had cervical cancer,
exposure to the HPV virus, and smoking (Chart 47-6).
Clinical Manifestations
There
are several different types of cervical cancer. Most cancers originate in
squamous cells, while the remainder are adenocarci-nomas or mixed adenosquamous
carcinomas. Adenocarcinomas begin in mucus-producing glands and are often due
to HPV in-fection. Most cervical cancers, if not detected and treated, spread
to regional pelvic lymph nodes, and local recurrence is not un-common. Early
cervical cancer rarely produces symptoms. If symptoms are present, they may go
unnoticed as a thin watery vaginal discharge often noticed after intercourse or
douching. When symptoms such as discharge, irregular bleeding, or bleed-ing
after sexual intercourse occur, the disease may be advanced. Advanced disease
should not occur if all women have access to gy-necologic care and avail
themselves of it. The nurse’s role in access and utilization is crucial and may
prevent the delay of detection of cervical cancer until the advanced stage.
In advanced cervical cancer, the vaginal discharge gradually increases and becomes watery and, finally, dark and foul-smelling from necrosis and infection of the tumor. The bleeding, which occurs at irregular intervals between periods (metrorrhagia) or after menopause, may be slight (just enough to spot the undergarments) and occurs usually after mild trauma or pressure (eg, intercourse, douching, or bearing down during defecation).
As the disease con-tinues, the bleeding may
persist and increase. Leg pain, dysuria, rec-tal bleeding, and edema of
extremities signal advanced disease.
As the
cancer advances, it may invade the tissues outside the cervix, including the
lymph glands anterior to the sacrum. In one third of patients with invasive
cervical cancer, the disease involves the fundus. The nerves in this region may
be affected, producing excruciating pain in the back and the legs that is
relieved only by large doses of opioid analgesic agents. If the disease progresses,
it often produces extreme emaciation and anemia, usually accom-panied by fever
due to secondary infection and abscesses in the ulcerating mass, and by fistula
formation. Because the survival rate for in situ cancer is 100% and the rate
for women with more advanced stages of cervical cancer decreases dramatically,
early de-tection is essential.
Assessment and Diagnostic Findings
Diagnosis
may be made on the basis of abnormal Pap smear re-sults, followed by biopsy
results identifying severe dysplasia (cer-vical intraepithelial neoplasia type
III [CIN III], high-grade squamous intraepithelial lesions [HGSIL] [also
referred to as HSIL], or carcinoma in situ; see below). HPV infections are
usu-ally implicated in these conditions. Biopsy results may indicate carcinoma
in situ. Carcinoma in situ is technically classified as se-vere dysplasia and
is defined as cancer that has extended through the full thickness of the
epithelium of the cervix, but not beyond. This is often referred to as
preinvasive cancer.
In its
very early stages, invasive cervical cancer is found mi-croscopically by Pap
smear. In later stages, pelvic examination may reveal a large, reddish growth
or a deep, ulcerating lesion. The patient may report spotting or bloody
discharge.
When
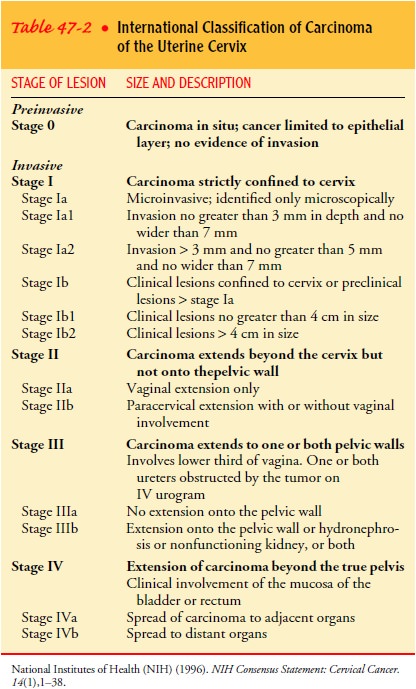
the patient has been diagnosed with invasive cervical cancer, clinical staging
estimates the extent of the disease so that treatment can be planned more
specifically and prognosis reasonably predicted. The International
Classification adopted by the International Federation of Gynecology and
Obstetrics and included in the NIH Consensus Conference on Cervical Cancer
(1996) (Table 47-2) is the most widely used staging system; the TNM (tumor,
nodes, and metastases) classification is also used in describing cancer stages.
In this system, T refers to the extent of the primary tumor, N to lymph node
involvement, and M to metastasis, or spread of the disease.
Signs
and symptoms are evaluated, and x-rays, laboratory tests, and special
examinations, such as punch biopsy and col-poscopy, are performed. Depending on
the stage of the cancer, other tests and procedures may be performed to
determine the ex-tent of disease and appropriate treatment. These tests include
dilation and curettage (D & C), computed tomography (CT) scan, magnetic
resonance imaging (MRI), intravenous urogra-phy, cystography, and barium x-ray
studies.
Medical Management
PRECURSOR OR PREINVASIVE LESIONS
When precursor lesions, such as low-grade squamous intra-epithelial lesion (LGSIL), which is also referred to as LSIL (CIN I and II or mild to moderate dysplasia), are found by colposcopy and biopsy, careful monitoring by frequent Pap smears or con-servative treatment is possible.
Conservative treatment may con-sist of monitoring, cryotherapy (freezing with nitrous
oxide), or laser therapy. A loop
electrocautery excision procedure (LEEP) may also be used to remove
abnormal cells. In this procedure, a thin wire loop with laser is used to cut
away a thin layer of cer-vical tissue. LEEP is an outpatient procedure usually
performed in a gynecologist’s office; it takes only a few minutes. Analgesia is
given before the procedure, and a local anesthetic agent is injected into the
area. This procedure allows the pathologist to examine the removed tissue
sample to determine if the borders of the tissue are disease-free. Another
procedure called a cone biopsy or conization
(removing a cone-shaped portion of the cervix) is per-formed when biopsy
findings demonstrate CIN III or HGSIL, equivalent to severe dysplasia and
carcinoma in situ.
If
preinvasive cervical cancer (carcinoma in situ) occurs when a woman has
completed childbearing, a hysterectomy is usually recommended. If a woman has
not completed childbearing and invasion is less than 1 mm, a cone biopsy may be
sufficient. Fre-quent re-examinations are necessary to monitor for recurrence.
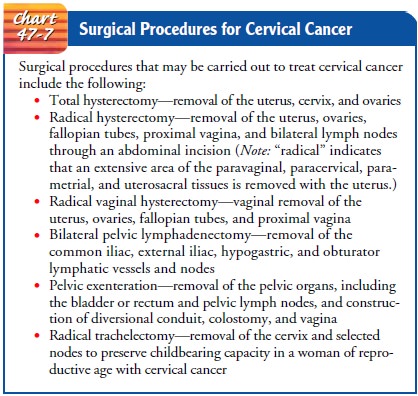
A
newly developed procedure called a radical trachelectomy is an alternative to
hysterectomy in women with cervical cancer who are young and want to have
children (Dargent, Martin, Sacchetoni & Mathevet, 2000). In this procedure
the cervix is gripped with retractors and pulled into the vagina until it is
visi-ble. The affected tissue is excised while the rest of the cervix and
uterus remain intact. A drawstring suture is placed to close the cervix.
Patients
who have precursor or premalignant lesions need re-assurance that they do not
have invasive cancer. However, the im-portance of close follow-up is emphasized
because the condition, if untreated for a long time, may progress to cancer.
Patients with cervical cancer in situ also need to know that this is usually a
slow-growing and nonaggressive type of cancer that is not expected to recur
after appropriate treatment.
INVASIVE CANCER
Treatment
of invasive cervical cancer depends on the stage of the lesion, the patient’s
age and general health, and the judgment and experience of the physician.
Surgery and radiation treatment (intra-cavitary and external) are most often
used. When tumor invasion is less than 3 mm, a hysterectomy is often
sufficient. Invasion ex-ceeding 3 mm usually requires a radical hysterectomy
with pelvic node dissection and aortic node assessment. Stage 1B1 tumors are
treated with radical hysterectomy and radiation. Stage 1B2 tu-mors are treated
individually because no single correct course has been determined, and many
variable options may be seen clini-cally (Chart 47-7). Frequent follow-up after
surgery by a gyne-cologic oncologist is imperative because the risk of
recurrence is 35% after treatment for invasive cervical cancer. Recurrence
usu-ally occurs within the first 2 years. Recurrences are often in the upper
quarter of the vagina, and ureteral obstruction may be a sign. Weight loss, leg
edema, and pelvic pain may be signs of lym-phatic obstruction and metastasis.
Radiation, which is often part of treatment to reduce recurrent disease, may be delivered by an external beam or by brachyther-apy (method by which the radiation source is placed near thetumor) or both. The field to be irradiated and dose of radiation are determined by stage, volume of tumor, and lymph node in-volvement. Treatment can be administered daily for 4 to 6 weeks followed by one or two treatments of intracavitary radiation. Inter-stitial therapy may be used when vaginal placement has become impossible due to tumor or stricture.
Platinum-based
agents are being used to treat advanced cervi-cal cancer. They are often used
in combination with radiation therapy, surgery, or both. Studies are ongoing to
find the best ap-proach to treat advanced cervical cancer. Vaginal stenosis is
a fre-quent side effect of radiation. Sexual activity with lubrication is
preventive, as is use of a vaginal dilator to avoid severe permanent vaginal
stenosis.
Some
patients with recurrences of cervical cancer are consid-ered for pelvic exenteration, in which a large
portion of the pelvic contents is removed. Unilateral leg edema, sciatica, and
ureteral obstruction indicate likely disease progression. Patients with these
symptoms have advanced disease and are not consid-ered candidates for this
major surgical procedure. Surgery is often complex because it is performed
close to the bowel, blad-der, ureters, and great vessels. Complications can be
considerable and include pulmonary emboli, pulmonary edema, myocardial
infarction, cerebrovascular accident, hemorrhage, sepsis, small bowel
obstruction, fistula formation, urinary obstruction of ileal conduit, bladder
dysfunction, and pyelonephritis, most often in the first 18 months. Vein
constriction must be avoided post-operatively. Patients with varicose veins or
a history of throm-boembolic disease may be treated prophylactically with
heparin. Pneumatic compression stockings are prescribed to reduce the risk for deep
vein thrombosis. Nursing care of these patients is complex and requires
coordination and care by experienced health care professionals. This is a
complex, extensive surgical procedure that is reserved for those with a high
likelihood of cure.
Related Topics