Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Nursing Process: The Patient With a Vulvovaginal Infection
NURSING
PROCESS: THE PATIENT WITH A VULVOVAGINAL INFECTION
Assessment
The
woman with vulvovaginal symptoms should be examined as soon as possible after
the onset of symptoms. She is instructed not to douche because doing so removes the vaginal discharge needed to
make the diagnosis. The area is observed for erythema, edema, excoriation, and
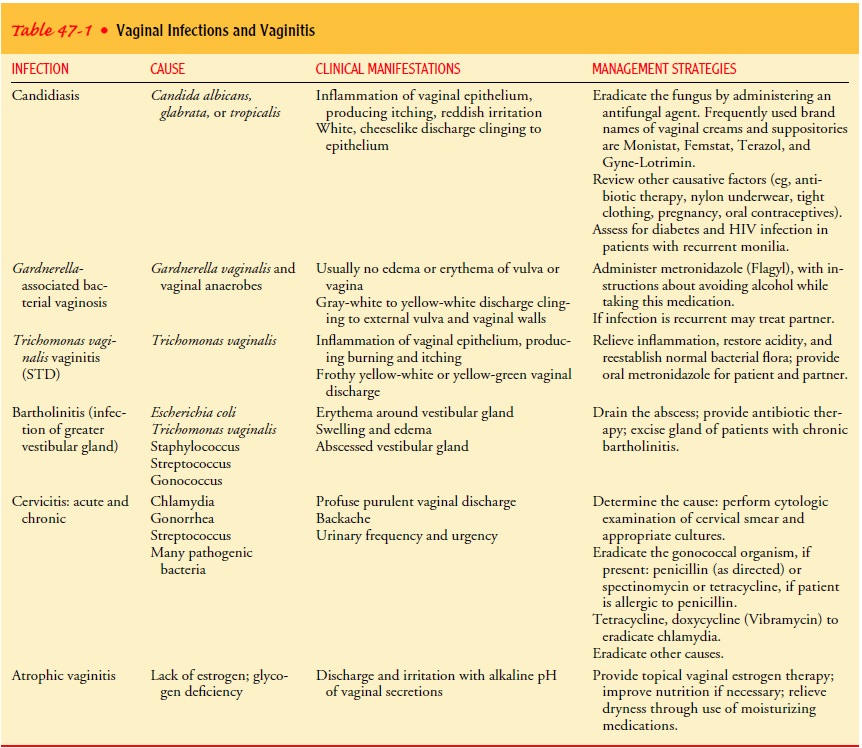
discharge. Each of the infection-producing or-ganisms produces its own
characteristic discharge and effect (see Table 47-1). The patient is asked to
describe any discharge and other symptoms, such as odor, itching, or burning.
Dysuria often occurs as a result of local irritation of the urinary meatus. A
uri-nary tract infection may need to be ruled out by obtaining a urine specimen
for culture and sensitivity testing.
The
patient is asked about the occurrence of factors that may contribute to
vulvovaginal infection:
·
Physical and chemical factors, such as constant
moisture from tight or synthetic clothing, perfumes and powders, soaps, bubble
bath, poor hygiene, and use of feminine hy-giene products
· Psychogenic factors (eg,
stress, fear of STDs, abuse)
· Medical conditions or
endocrine factors, such as a predis-position to vulvar involvement in a patient
who has diabetes or is elderly
· Use of medications such
as antibiotics, which may alter the vaginal flora and allow an overgrowth of
monilial organisms
· New sex partner,
multiple sex partners, previous vaginal infection
The
patient is also asked about other factors that could con-tribute to infection,
including hygiene practices (tampons, douching), use or nonuse of condoms, and
use of chemicals such as nonoxynol-9 with barrier methods of birth control.
The
nurse may prepare a vaginal smear (wet mount) to assist in diagnosing the
infection. A common method for preparing the smear is to collect vaginal
secretions with an applicator and place the secretions on two separate glass
slides. A drop of saline solu-tion is added to one slide and a drop of 10%
potassium hydrox-ide is added to another slide for examination under a
microscope. If bacterial vaginosis is present, the slide with normal saline
solu-tion added shows epithelial cells dotted with bacteria (clue cells). If Trichomonas species is present, small
motile cells are seen. In the presence of yeast, the potassium hydroxide slide
reveals typi-cal characteristics. Discharge associated with bacterial vaginosis
produces a strong odor when mixed with potassium hydroxide. This is called a positive
“whiff test.” Testing the pH of the dis-charge with Nitrazine paper assists in
proper diagnosis.
Diagnosis
NURSING DIAGNOSES
Based
on the nursing assessment and other data, the patient’s major nursing diagnoses
may include the following:
· Discomfort related to
burning, odor, or itching from the in-fectious process
· Anxiety related to
stressful symptoms
· Risk for infection or
spread of infection
· Deficient knowledge
about proper hygiene and preventive measures
Planning and Goals
The
major goals for the patient may include relief of discomfort, reduction of
anxiety related to stress symptoms, prevention of re-infection or infection of
sexual partner, and acquisition of knowl-edge about methods for preventing
vulvovaginal infections and managing self-care.
Nursing Interventions
RELIEVING DISCOMFORT
Treatment
with the appropriate medication usually relieves dis-comfort. Sitz baths are
occasionally recommended. Use of corn-starch powder may relieve discomfort and
skin irritation.
REDUCING ANXIETY
Although
vulvovaginal infections are upsetting and require treat-ment, they are not
life-threatening. The patient who experiences such an infection, however, may
be anxious and fearful about the significance of the symptoms and possible
causes. Explaining the cause of symptoms may reduce anxiety related to fear of
a more serious illness. Discussing ways to help prevent vulvovaginal
in-fections may help the patient adopt specific strategies to decrease
infection and the related symptoms.
PREVENTING REINFECTION OR SPREAD OF INFECTION
There
is a risk of another episode of the same infection or spread of the infection
to sexual partners. The patient needs to be in-formed about these risks and the
importance of adequate treat-ment of herself and her partner, if indicated.
Other strategies to prevent persistence or spread of infection include
abstaining from sexual intercourse when infected, treatment of sexual partners,
and minimizing irritation of the affected area. When medications such as
antibiotic agents are prescribed for any infection, the nurse instructs the
patient about the usual precautions related to using these agents. If vaginal
itching occurs, the patient can be re-assured that this is usually not an
allergic reaction but may be a yeast or monilial infection resulting from
altered vaginal bacteria. Treatment for monilial infection is prescribed.
Another
goal of treatment is to reduce tissue irritation caused by scratching or
wearing tight clothing. The area needs to be kept clean by daily bathing and
adequate hygiene after voiding and defecation. The use of a cool-air hairdryer
and application of top-ical corticosteroids may be useful to keep the area dry
and mini-mize irritation.
When
teaching the patient about medications such as sup-positories and devices such
as applicators to dispense cream or ointment, the nurse may demonstrate the
procedure by using a plastic model of the pelvis and vagina. The nurse should
also stress the importance of hand washing before and after each
ad-ministration of medication. To prevent the medication from es-caping from
the vagina, the patient should recline for 30 minutes after it is inserted, if
possible. The patient is informed that seep-age of medication may occur, and
the use of a perineal pad may be helpful.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Vulvovaginal
conditions are treated on an outpatient basis, unless the patient has other
medical problems. Patient teaching, tact, and reassurance are important aspects
of nursing care. Women may ex-press embarrassment, guilt, or anger and may be
concerned that the infection may be serious (causing infertility) or that it
may have been acquired from a sex partner. In some instances, treat-ment plans
include the partner.
In
addition to reviewing ways of relieving discomfort and pre-venting reinfection,
the nurse assesses each patient’s learning needs relative to the immediate
problem. The patient needs to know the characteristics of normal as opposed to
abnormal dis-charge. Questions often arise about douching. Normally, douch-ing
and use of feminine hygiene sprays are unnecessary because daily baths or
showers and proper hygiene after voiding and defe-cating keep the perineal area
clean. Douching tends to eliminate normal flora, reducing the body’s ability to
ward off infection. In addition, repeated douching may result in vaginal
epithelial breakdown and chemical irritation and has been associated with other
pelvic disorders.
Therapeutic
douching, however, may be recommended and prescribed to reduce unpleasant,
abnormal odors; to remove ex-cessive discharge; to change the pH (eg, vinegar
douches); and to serve as an antiseptic irrigating solution. The procedure is
re-viewed with the patient, as is the care and cleaning of equipment so that it
is properly disinfected.
In the
case of recurrent yeast infections, the perineum should be kept as dry as
possible. Loose-fitting cotton instead of tight-fitting synthetic,
nonabsorbent, heat-retaining underwear is rec-ommended. The patient is
instructed to perform a monthly inspection of the vulvar region for changes.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Experiences reduced
discomfort
a)
Cleans the perineum as instructed
b)
Reports that itching is relieved
c)
Maintains urine output within normal limits and
with-out dysuria
2) Experiences relief of
anxiety
3) Remains free from
infection
a)
Has no signs of inflammation, pruritus, odor, or
dysuria
b)
Notes that vaginal discharge appears normal (thin,
clear, not frothy)
4) Participates in self-care
a)
Takes medication as prescribed
b)
Wears absorbent underwear
c)
Avoids unprotected sexual intercourse
d)
Douches only as prescribed
Related Topics