Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Nursing Process: The Patient With a Genital Herpesvirus Infection
NURSING
PROCESS: THE PATIENT WITH A GENITAL HERPESVIRUS INFECTION
Assessment
The
health history and a physical and pelvic examination are important in
establishing the nature of the infectious condi-tion. Additionally, the patient
is assessed for risk for STDs. The perineum is inspected for painful lesions.
Inguinal nodes are assessed because they often are enlarged and tender during
an oc-currence of HSV.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
· Acute pain related to
the genital lesions
· Risk for infection or
spread of infection
· Anxiety related to the
diagnosis
· Deficient knowledge
about the disease and its management
Planning and Goals
The
major goals for the patient may include relief of pain and dis-comfort, control
of infection and its spread, relief of anxiety, knowledge of and adherence to
the treatment regimen and self-care, and knowledge about implications for the
future.
Nursing Interventions
RELIEVING PAIN
The
lesions should be kept clean, and proper hygiene practices are advocated. Sitz
baths ease discomfort. Clothing should be clean, loose, soft, and absorbent.
Aspirin and other analgesics are usually effective in controlling pain.
Occlusive ointments and powders are avoided because they prevent the lesions
from drying.
If
there is considerable pain and malaise, bed rest may be re-quired. The patient
is encouraged to increase fluid intake, to be alert for possible bladder
distention, and to contact her primary health care provider immediately if she
cannot void because of discomfort. Painful voiding may occur if urine comes in
contact with the herpes lesions. Discomfort with urination can be re-duced by
pouring warm water over the vulva during voiding or by sitz baths. When oral
acyclovir or other antiviral agents are prescribed, the patient is instructed
about when to take the med-ication and what side effects to note, such as rash
and headache. Rest, fluids, and a nutritious diet are recommended to promote
recovery.
PREVENTING INFECTION AND ITS SPREAD
The
risk of reinfection and spread of infection to others or to other structures of
the body can be reduced by hand washing, use of bar-rier methods with sexual
contact, and adherence to prescribed medication regimens. Avoidance of contact
when obvious lesions are present does not eliminate the risk because the virus
can be shed in the absence of symptoms, and lesions may not be visible to the
woman. Avoiding stress, sunburn, and other stress-producing situations may
decrease the episodes of recurrence.
RELIEVING ANXIETY
Concern
about the presence of herpes infection, future occur-rences of lesions, and the
impact of the infection on future rela-tionships and childbearing may cause
considerable anxiety in the patient. The nurse can be an important support,
listening to the patient’s concerns and providing information and instruction.
The patient may be angry with her partner if her partner is the probable source
of the infection. She may need assistance and support in discussing the
infection and its implications with her current sexual partner and in future
sexual relationships. The nurse can refer the patient to a support group to assist
in coping with the diagnosis.
INCREASING KNOWLEDGE ABOUT THE DISEASE AND ITS TREATMENT
Patient
teaching is an essential part of nursing care of the patient with a genital
herpes infection. This includes an adequate expla-nation about the infection
and how it is transmitted, manage-ment and treatment strategies, strategies to
minimize spread of infection, the importance of adherence to the treatment
regimen, and self-care strategies. Because of the increased risk of HIV and
other STDs in the presence of skin lesions, an important part of patient
education involves instructing the patient to protect her-self from exposure to
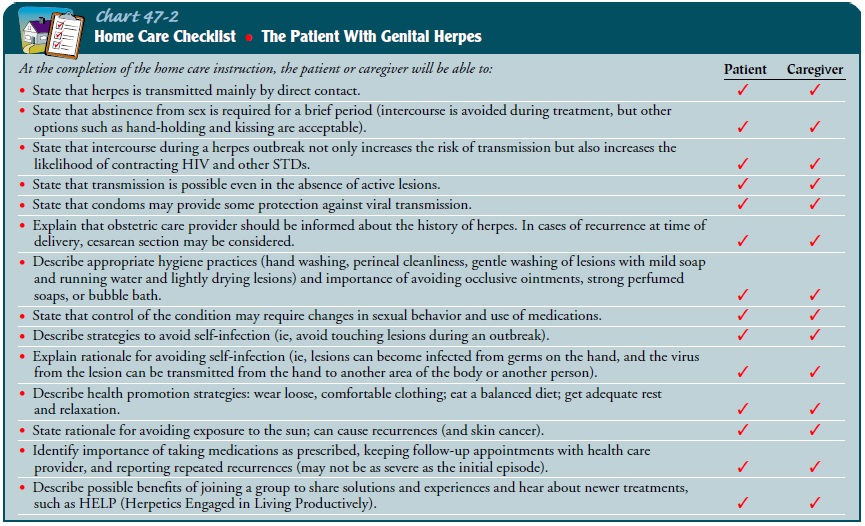
HIV and other STDs. Further details are included in Chart 47-2.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Genital
herpes causes physical pain and emotional distress. Usu-ally, the patient is
upset on learning the diagnosis. Therefore, when counseling the patient, the
nurse should explain the causes of the condition and the manner in which it can
be managed. Questions are encouraged because they may indicate that the
pa-tient is receptive to learning.
The
nurse can provide reassurance that the lesions will heal and that recurrences
can be minimized by adopting a healthful lifestyle and by taking prescribed
medications. Self-care measures for the person with genital herpes appear in
Chart 47-2.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Experiences a reduction
in pain and discomfort
2) Keeps infection under
control
a)
Demonstrates proper hygiene techniques
b)
Takes medication as prescribed
c)
Consumes adequate fluids
d)
Adopts healthy lifestyle (diet, adequate fluid
intake, safer sex practices, stress management)
3) Uses strategies to
reduce anxiety
a)
Verbalizes issues and concerns related to genital
herpes infection
b)
Discusses strategies to deal with issues and
concerns with current and future sexual partner
c)
Initiates contact with support group if indicated
4) Demonstrates knowledge
about genital herpes and strate-gies to control and minimize recurrences
a)
Identifies methods of transmission of herpes
infection and strategies to prevent transmission to others
b)
Discusses strategies to reduce recurrence of
lesions
c)
Takes medications as prescribed
d)
Reports no recurrence of lesions
Related Topics