Chapter: Medical Surgical Nursing: Management of Patients With Female Reproductive Disorders
Fistulas of the Vagina - Structural Disorders
Structural Disorders
FISTULAS
OF THE VAGINA
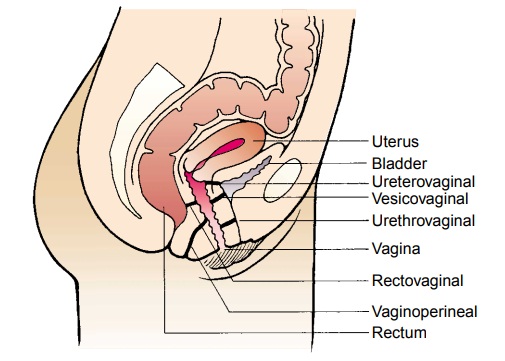
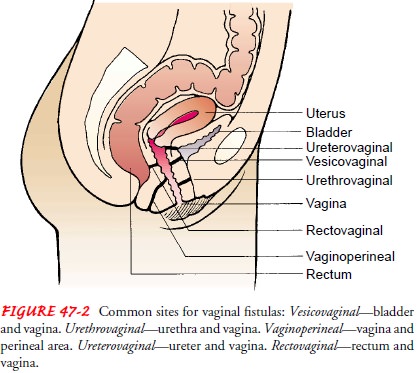
A fistula is an abnormal, tortuous
opening between two internal hollow organs or between an internal hollow organ
and the exte-rior of the body. The name of the fistula indicates the two areas
that are connected abnormally: a vesicovaginal fistula is an open-ing between
the bladder and the vagina, and a rectovaginal fistula is an opening between
the rectum and the vagina (Fig. 47-2). Fis-tulas may be congenital in origin.
In adults, however, breakdown usually occurs because of tissue damage resulting
from injury sus-tained during surgery, vaginal delivery, radiation therapy, or
dis-ease processes such as carcinoma.
Clinical Manifestations
Symptoms depend on the specific defect. For example, in the pa-tient with a vesicovaginal fistula, urine escapes continuously into the vagina. With a rectovaginal fistula, there is fecal incontinence, and flatus is discharged through the vagina. The combination of fecal discharge with leukorrhea results in malodor that is difficult to control.
Assessment and Diagnostic Findings
A
history of the symptoms experienced by the patient is impor-tant to identify
the structural alterations and to assess the impact of the symptoms on the
patient’s quality of life. In addition, the use of methylene blue dye helps
delineate the course of the fistula. In vesicovaginal fistula, the dye is
instilled into the bladder and appears in the vagina. After a negative
methylene blue test result, indigo carmine is injected intravenously; the
appearance of the dye in the vagina indicates a ureterovaginal fistula.
Cystoscopy or intravenous pyelography may then be used to determine the exact
location.
Medical Management
The
goal is to eliminate the fistula and to treat infection and ex-coriation. A
fistula may heal without surgical intervention, but surgery is often required.
If the primary care provider determines that a fistula will heal without
surgical intervention, care is planned to relieve discomfort, prevent infection,
and improve the patient’s self-concept and self-care abilities. Measures to
effect healing in-clude proper nutrition, cleansing douches and enemas, rest,
and administration of prescribed intestinal antibiotic agents. A recto-vaginal
fistula heals faster when the patient eats a low-residue diet and when the
affected tissue drains properly. Warm perineal irri-gations and controlled
heat-lamp treatments promote healing.
Sometimes
a fistula does not heal on its own and cannot be surgically repaired. In this
situation care must be planned and implemented on an individual basis.
Cleanliness, frequent sitz baths, and deodorizing douches are required, as are
perineal pads and protective undergarments. Meticulous skin care is nec-essary
to prevent excoriation. Applying bland creams or lightly dusting with
cornstarch may be soothing. Additionally, attend-ing to the patient’s social
and psychological needs is an essential aspect of care.
If the
patient will have a fistula repaired surgically, preopera-tive treatment of any
existing vaginitis is important to ensure suc-cess. Usually, the vaginal
approach is used to repair vesicovaginal and urethrovaginal fistulas; the
abdominal approach is used to re-pair fistulas that are large or complex.
Fistulas that are difficult to repair or that are very large may require
surgical repair with a uri-nary or fecal diversion.
Because
fistulas usually are related to obstetric, surgical, or radi-ation trauma,
occurrence in a patient without previous vaginal delivery or a history of
surgery must be evaluated carefully. Crohn’s disease or lymphogranuloma
venereum may be the cause.
Despite
the best surgical intervention, fistulas may recur. After surgery, medical
follow-up continues for at least 2 years to mon-itor for a possible recurrence.
Related Topics