Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Tiredness in Pregnancy
TIREDNESS IN PREGNANCY
History
A
27-year-old woman attends the antenatal clinic at 19 weeks’ gestation in her first ongoing pregnancy, having had a termination aged 22 years.
She is now happy to be pregnant.
She booked with the midwife at 8 weeks and has had normal
booking bloods, blood pressure
and ultrasound scan.
She
experienced nausea and vomiting until
14 weeks’ gestation. This has now settled but she
remains very tired
and feels that she is gaining excessive weight in the pregnancy. She also
feels cold for much of the time,
which surprises her as she understood that pregnant
women tend to feel hot.
Examination
The
woman appears lethargic and of low mood. Her blood pressure
is 115/68 mmHg and heart rate 58/min. Abdominal examination is unremarkable, with the fundus
palpable at the umbilicus.
Questions
·
What is the diagnosis and what features
will you look for on examination?
·
What are the implications for the mother
and baby in pregnancy?
·
How should the condition be managed?
ANSWER
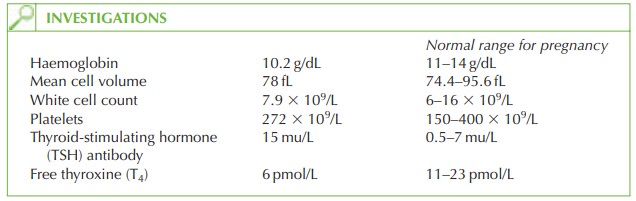
The
full blood count shows mild anaemia, with relatively low mean cell volume. This is
not significant enough to account
for the symptoms described.
The
thyroid function tests confirm the clinical diagnosis
of hypothyroidism. There is no history of radioactive iodine
or surgical treatment, and Hashimoto’s thyroiditis is unlikely as there
has been no history of a hyperthyroid episode. This case therefore probably represents idiopathic myxoedema.
The
symptoms of tiredness, cold intolerance and weight gain may all relate to the hypo-
thyroidism. In addition she
may report dry skin, coarse hair, depression or constipation.
Examination may reveal relative
bradycardia, blunted deep tendon reflexes or goitre.
Implications for the pregnancy and management
Hypothyroidism occurs
in approximately 1 in 100 pregnancies, but this case
is unusual to be diagnosed in pregnancy.
Myxoedematous coma is a very rare consequence of hypothyroidism, associated with a high mortality rate. It is a medical
emergency managed by supportive care and thyroxine supplementation. In the absence
of a coma, thyroxine replacement is still needed
and should be titrated
to the TSH and T4 results.
In
pregnancy, the thyroxine
requirement may increase,
and the TSH and T4 should be checked every
trimester once a maintenance regime
has been established. The aim should be to keep the TSH less than 5 mu/L.
(Although the thyroid-binding globulin increases in pregnancy, there is a compensatory
rise in tri-iodothyronine (T3) and T4 production such that the levels of free T3 and free T4 remain similar to
non-pregnant values.)
The fetus
Untreated hypothyroidism is associated with an increased risk of infertility, miscarriage, stillbirth and pre-eclampsia. The fetal and
neonatal outcome is generally good
in women diagnosed and
treated appropriately. Anti-TSH antibodies may very
rarely cross the
pla- centa and cause
neonatal hypothyroidism, and
this should be suspected if there are
signs of neonatal goitre.
Related Topics