Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Glucose Tolerance Test
GLUCOSE TOLERANCE TEST
History
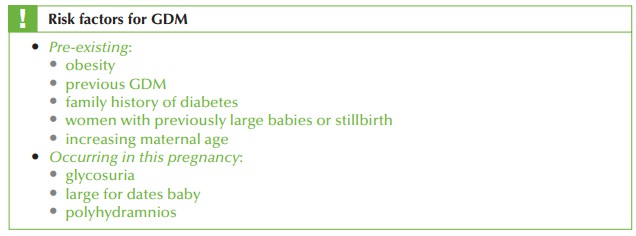
A woman attends the antenatal day assessment unit to discuss the result of her glucose tolerance test. She is 42 years old and this is her sixth pregnancy. She has previously had three Caesarean sections, one early miscarriage and a termination of pregnancy. All book- ing tests were normal as were her 11–14-week and anomaly ultrasound scans.
The
woman is of Indian ethnic
origin but was
born and has
always lived in the UK.
She is now 26 weeks’ gestation
and her midwife arranged a glucose tolerance
test because of a
family history of type 2 diabetes (her father and paternal aunt).
Examination
The
body mass index
(BMI) is 31 kg/m2. Blood pressure
is 146/87 mmHg.
The symphysio- fundal height
is 29 cm and the
fetal heart rate
is normal on auscultation.
Questions
·
What is the diagnosis and on what criteria can this be made?
·
What are the principles of management for this patient?
ANSWER
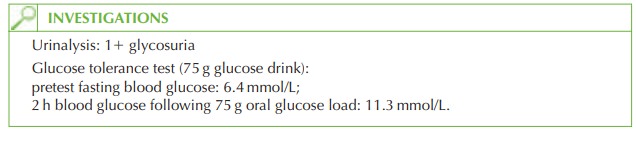
The
diagnosis is of gestational diabetes
mellitus (GDM) and is based
on the 2 h glucose concentration exceeding
11.1 mmol/L (World Health Organization (WHO) criteria). The diagnosis may also be made if the fasting
blood glucose exceeds
7.8 mmol/L, in which
case a formal glucose tolerance test would not
have been necessary. Transient glycosuria
is common in pregnancy and
may occur after
a glucose-rich drink
or snack. Therefore the urinalysis alone is unhelpful in the assessment of this woman.
GDM
occurs in up to 3 per cent of the pregnant population depending on the ethnic diver- sity of the specific population. In some
cases it may
be the first
presentation of previously undiagnosed diabetes.
The importance of the diagnosis
relates to the effect on the mother and fetus.
Effects on the fetus:
·
fetal macrosomia
·
polyhydramnios
·
neonatal hypoglycaemia
·
neonatal respiratory distress syndrome
·
increased stillbirth rate
Effects on the mother:
·
increased risk of traumatic
delivery (e.g. shoulder
dystocia)
·
increased Caesarean section risk
·
increased risk of developing GDM in subsequent pregnancies
·
50
per cent increased risk of developing type 2 diabetes
within 15 years
Management principles
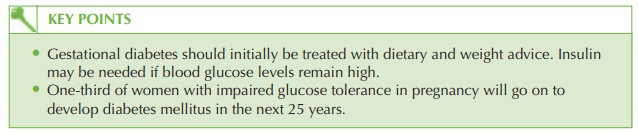
· Optimal control of maternal blood glucose minimizes the chance of fetal compli- cations. This needs the multidisciplinary input of a diabetologist, specialist diabetes nurse, dietitian, specialist midwife and obstetrician.
·
Dietary advice and counselling are the initial
interventions (reduced fat and carbo- hydrate intake with weight control).
·
Blood glucose monitoring at home should be initiated
with pre- and
post-prandial levels
at each meal.
·
Oral hypoglycaemics are contraindicated in pregnancy.
·
If
blood glucose measurements are repeatedly high,
insulin should be commenced.
·
The
fetus should be monitored with regular ultrasound scans for growth and liquor volume (polyhydramnios being a sign of fetal polyuria
secondary to excessive glucose level).
·
Delivery should be planned
by 40 weeks, but Caesarean section should be performed
for obstetric indications only.
·
Sliding-scale insulin should be initiated in labour for women on insulin.
·
The
insulin can be stopped immediately postpartum as normal
glucose homeostasis returns
rapidly after delivery.
·
The
fetus should be carefully monitored for neonatal hypoglycaemia.
·
The
mother should have a repeat
glucose tolerance test 6 weeks
postpartum to rule out
pre-existing diabetes.
Related Topics