Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Group B Streptococcus
GROUP B STREPTOCOCCUS
History
You are asked
to see a woman in the antenatal assessment unit. She is gravida
4, para 1, having had a normal
vaginal delivery 3 years ago, a first-trimester miscarriage and two first-trimester terminations.
She
is currently 26 weeks’ gestation. One week ago she was seen because
she experienced vaginal bleeding. At the time
a small cervical ectropion had been
noticed and as the bleed had occurred postcoitally, it was assumed
likely to be secondary to the ectropion.
However, as per protocol, she had vaginal
and endocervical swabs
sent and a full blood count and group and save sample
requested.
Questions
·
How would you interpret these results?
·
How
would you manage
the pregnancy and delivery in light of these results?
Answer:
The key results are
·
mild anaemia
·
group B streptococcus carrier
·
candida.
The
anaemia is mild for pregnancy and as the mean cell volume is low, suggesting iron deficiency, it may be treated with
ferrous sulphate 200
mg twice daily,
with repeat haemo- globin after 4 weeks.
She should also
be advised about
an appropriate iron-rich diet (e.g. meat, lentils, spinach).
Candida organisms are present
very commonly in the vagina,
particularly in pregnancy. This should be treated
(with vaginal clotrimoxazole) only if the woman is symptomatic
(itching or lumpy discharge).
Group B streptococcus (GBS)
GBS
(Streptococcus agalactiae) colonization occurs in 25 per
cent of women
at some stage during their pregnancy. In this case
the finding of GBS may
relate to the
presenting symp- tom of bleeding, but
is most likely
to be an incidental finding. This is the
most important result as there is a risk
of GBS to the baby
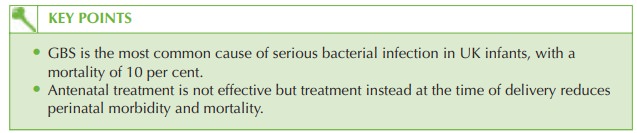
with an incidence of 1 in 2000 neonates being infected, with 6 per cent mortality.
In the UK,
universal screening for
GBS has not
been shown to be effective in reducing
neonatal death.
Management
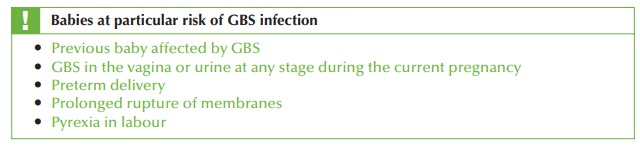
Antenatal treatment does not seem to reduce the neonatal risk (perhaps because of recoloniza- tion). However measures are taken to reduce transmission to the baby at the time of delivery:
·
intravenous penicillin (or clindamycin or erythromycin if allergic) should always be given to the mother in labour
·
neonatal care depends on the clinical
scenario but may include:
·
observation of the baby for up to 5 days postpartum for signs of sepsis
·
consideration of culture of the baby for evidence
of infection (ear,
nose, axilla)
·
intravenous antibiotics until culture
results confirm no evidence of infection.
Related Topics