Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Postpartum Chest Pain
POSTPARTUM CHEST PAIN
History
A
32-year-old Sri Lankan woman presents complaining of chest pain, neck tightness
and shortness of breath
3 weeks after delivery.
The symptoms have come on gradually
over the last 2 days and are now severe. She feels as if she cannot breathe and thinks she is going to die.
The
pain is heavy
and stabbing and
is constant though
worse when she
lies down and
tries to sleep. The pain is not pleuritic and she says it radiates
up into her neck. She does not have a cough or haemoptysis.
The
neck tightness is all over
the neck but
especially anteriorly, and
is related to the
difficulty breathing. There is no photophobia or fever.
The
breathing difficulty occurs
predominantly when she
is trying to sleep or is sleeping – it has woken
her several times
during the night.
She is now terrified of going to sleep and is
actively stopping herself
from doing so as she is certain
that she will die if she does.
Prior to this she
has always been
fit and well
with no previous medical history reported.
The
pregnancy was uneventful and she was admitted in spontaneous labour
at 40 weeks. Cervical dilatation was
slow and contractions were therefore augmented with syntocinon.
Once fully dilated she had pushed for 90 min and subsequently underwent ventouse deliv- ery of a healthy female infant.
She
had some difficulty establishing breast-feeding and bonding with the baby and was finally discharged home on day four following delivery.
Since going home she has stopped breast-feeding but is finding it difficult to sleep even when the baby is sleeping.
She
has lived in the UK for 18 months but her husband
has been here for 6 years.
Currently her mother
is also staying
with them to help with
the baby. Both the
woman and her mother
speak very little
English and the husband is interpreting.
Examination
She
is thin and
quiet, with little
eye contact. When
talking about the
baby she is non-
responsive and she
does not look
at or touch the baby
during the consultation. Her blood pressure is 108/62 mmHg
and heart rate 90/min. She is apyrexial. There are no signs of anaemia, cyanosis or oedema.
Chest and cardiac
examination are normal
and the uterus is just palpable in the lower abdomen.
Questions
·
What is the likely diagnosis?
·
What further questions would you
wish to ask and what are the principles of management?
Answer:
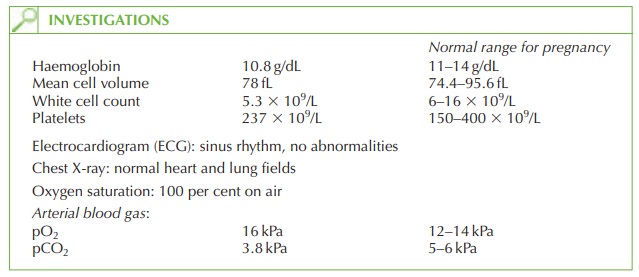
The
symptoms initially sound possibly cardiac or respiratory in origin.
However, the story does not fit with any
specific disease and
the examination and investigations are
all normal. The absolute
fear of sleeping
is an important piece of information as is the
reported affect.
This woman is suffering
from postnatal psychosis. This occurs in 1 in 500 women with
onset in the first 6 weeks post delivery. The commonest symptoms
are delusions (e.g.
the thought that she is going to die) and hallucinations.
The condition should be
distinguished from the two other main psychological/psychiatric postnatal
conditions.
·
Post-partum blues:
·
tearfulness
·
fatigue
·
anxiety over their own or the baby’s health
·
feelings of inability to cope
This is very common
(probably affecting approximately half of mothers) usually after the third postnatal day, and resolves
spontaneously over a few days.
·
Post-partum depression:
·
low
mood
·
crying
·
anxiety over the baby’s health
·
feelings of guilt towards
the baby
·
panic attacks
·
excessive tiredness
·
poor appetite
This occurs in 10 per
cent of women,
any time up to 6 months following delivery. It should be treated seriously with suicide risk assessment and antidepressant medication as well as social and practical support.
Further questioning
A
trained interpreter should
be sought rather
than the husband
who is involved in this case and may find it difficult
to translate or address sensitive
issues.
The
woman should be asked for any previous
personal or family
history of mental
illness or psychiatric treatment. She should then be asked
more probing questions. How is her mood
and appetite? Does
she feel depressed? Does she have
fears of harming
herself?
Her
relationship and attitudes
to the baby are important
– how does she feel about the baby?
Is she finding the baby easy? Does she feel that the baby is healthy? Does she have any
negative thoughts toward
the baby such
that it is bad or evil? Does
she feel she
might harm the baby?
Suicide is now the commonest cause
of indirect maternal
death, and non-English-speaking immigrants are
particularly at risk
as well as those aged
over 30 years,
with previous psychotic history,
poor social support
or traumatic delivery. This woman has three such risk factors.
The
diagnosis should always
be considered when symptoms do not appear
to be backed up by the examination or investigations. Sometimes delusional symptoms or hallucin-
ations are not elicited because
the doctor fails
to take a thorough history.
Management
Disease progression can be acute and this woman
needs immediate referral
to a mother and baby psychiatric unit for assessment and treatment. Depending
on her feelings of harm towards herself or others,
this may need to be under the Mental Health Act. Antidepressants,
antipsychotics and possibly
sedation may be needed. The baby may be at risk from neglect or harm secondary to the psychosis, so close supervision and support is essential.
Recovery is expected within 2 months but repeat pregnancy and non-pregnancy-related
episodes are common.
Related Topics