Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Bleeding in Pregnancy
BLEEDING IN PREGNANCY
History
You are asked to review a nulliparous woman
who has presented with vaginal bleeding
at 39 weeks + 5 days’
gestation. Booking blood
pressure was 123/72
mmHg. Her last midwife
visit was 10 days ago when blood pressure
was 130/76 mmHg.
This evening she noticed
a small ‘gush’ of blood and discovered a bright red stain in her
underclothes. She denies actual abdominal pain but reports some intermittent
lower abdominal discomfort. The
baby has been
moving normally during
the day.
Examination
She
is warm and well perfused.
Her blood pressure
is 158/87 mmHg and heart rate 84/min. The symphysiofundal height is 36 cm and the fetus is cephalic with 3/5 palpable
abdomin- ally. Moderate
uterine tenderness is noted. The uterus is soft but during the palpation two moderate uterine tightenings are noted. On speculum examination the cervical os is closed and there is a moderate amount of vaginal
blood.
Questions
·
What is the diagnosis?
·
How should this woman be managed?
Answer:
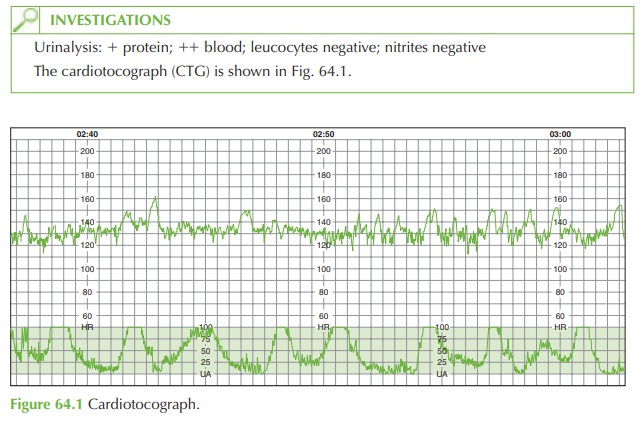
The
diagnosis is of placental abruption
in view of the bleeding,
uterine tenderness and irritability. CTG is reassuring at present with baseline 130 beats/min, normal
variability, several accelerations and no decelerations. Regular uterine activity
is demonstrated on the
tocograph.
A ‘show’ can
be ruled out,
as the blood
is fresh rather
than mucus-like and
dark. Placenta praevia would
have been detected
at the anomaly scan, and bleeding placenta
praevia is typically painless. She has no features suggesting infection, and vasa praevia bleeding would normally occur with rupture of membranes. Placental abruption is supported by the history of fresh bleeding
and uterine irritability and the associated high blood pres- sure and proteinuria (pre-eclampsia is a cause of abruption).
Placental abruption may be major with
catastrophic haemorrhage or, as in this
case, be less dramatic. However, caution should
be maintained for
two reasons: first,
a small bleed may herald a larger bleed. Second,
although some bleeding
is revealed, there may be a
more significant concealed bleed. Pregnant women
may not show any signs
of hypo- volaemic shock until a large amount of blood has been lost.
Management
Women with APH should always
be admitted for observation. Initial
management for this woman includes intravenous access,
group and save,
full blood count
and clotting profile. Urea, electrolytes and urate
should be sent,
looking for abnormalities associated with pre- eclampsia; 24-h urine collection for proteinuria is not indicated in this case
as induction of labour
is already indicated on clinical grounds.
Blood pressure should
be repeated at regular intervals and antihypertensives commenced if indicated.
Induction of labour may increase the chance of operative intervention, but the risk of
expectant management is that sudden
and catastrophic further
haemorrhage may occur. As the
woman is over 37 weeks,
there is little
risk to the fetus of prematurity from induction.
Related Topics