Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: HIV in Pregnancy
HIV IN PREGNANCY
History
A
36-year-old Nigerian woman
who has lived
in the UK for 8 years attends
the antenatal clinic. She had a daughter by spontaneous vaginal
delivery at term 12 years
ago and a termination of pregnancy 9 years ago. She and her partner
have now been trying to con-
ceive for 4 years.
Her
last menstrual period
was 11 weeks ago. There is no significant gynaecological his-
tory and last smear test was normal
2 years ago.
The
woman saw the midwife for a routine
antenatal booking appointment a week ago and
no relevant past medical history
was reported. All routine booking
blood tests were accepted.
Questions
·
What is the diagnosis?
·
What is the next stage in management?
·
What are the important points in the
management of the
pregnancy in view
of the diagnosis?
Answer:
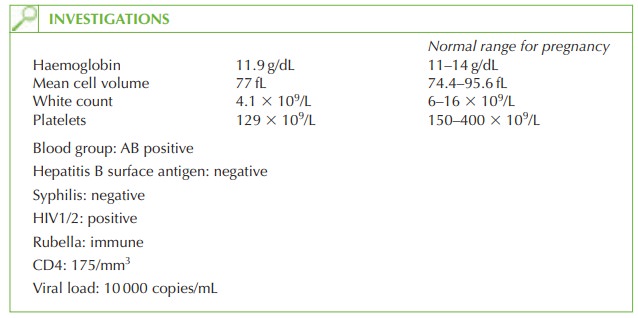
The diagnosis is human immunodeficiency virus (HIV) infection. HIV screening in pregnancy is recommended for all women in the UK and the latest reported
incidence was approxi- mately 0.5 per cent in inner London
and less than 0.1 per cent for the rest of the UK. It is particularly prevalent in women from Africa (1.91 per cent compared
with <0.5 per cent from all other areas).
The vast majority
of paediatric HIV cases in the UK result from mother-to-child transmission.
The
low CD4 count
suggests that this woman needs
to commence treatment, but there are no AIDS-defining illnesses in the history.
Immediate management
The
woman needs to be informed
of the diagnosis and a second different diagnostic test
performed to confirm the diagnosis. Most women choose
to continue with their pregnan- cies, but she may still wish to consider
the option of termination, as she is only 11 weeks’ gestation. She needs urgent
referral to the genitourinary medicine
specialist for further examination and investigation for any HIV complications. She will need to start Pneumocystis carinii prophylaxis in view of the low
CD4 count, and
she will also
need antiretroviral
treatment in view of the significant viral
load.
Psychological counselling in relation to the diagnosis, the implications for
her, her part- ner and her offspring (the fetus and her 12-year-old daughter) is very important.
Management of the pregnancy
Pregnancy does not adversely affect the HIV
disease process. The
important consideration is
therefore the prevention of transmission from mother to child. Untreated,
approxi- mately 25 per
cent of infants
of mothers with
HIV will become
infected. With appropriate measures, this is reduced
to less than 5 per cent:
·
elective Caesarean section
·
avoidance of breast-feeding
·
intravenous zidovudine to the mother prior to delivery
(ideally for 4 h)
·
oral zidovudine to the neonate for 6 weeks postnatally.
·
More recently, vaginal delivery
has been shown
to have no effect on infant infection if the viral load is undetectable at the time of delivery.
Confidentiality is of paramount importance for women
diagnosed antenatally with HIV, and
coding systems in the hand-held obstetric notes can be helpful
in alerting other medical staff to the diagnosis.
Related Topics