Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Illegal Drug Use in Pregnancy
ILLEGAL DRUG USE IN PREGNANCY
History
A
19-year-old woman is referred to the antenatal clinic by her general practitioner (GP). She is currently 22 weeks’ gestation in her second
pregnancy. She had a son by normal vaginal delivery 18 months
ago, who was taken into social services
care initially and now
lives with his grandparents (the father’s parents).
Since then, the woman has been
having very infrequent periods and only discovered she was pregnant
when she attended the emergency department with a presumed
urinary tract infection 2 weeks ago. At that stage abdominal palpation revealed a mass, and
ultrasound scan confirmed the singleton
gestation.
The
GP letter informs
that the woman has been a user of crack cocaine and heroin
in the past but that she has been on a methadone
replacement programme for the last 8
weeks. The current
prescribed regime is 60 mL methadone, which
she collects daily
from the pharmacist.
The
woman reports that she still
injects street heroin
several times per week but has not used
crack cocaine for several months.
She says that she drinks
minimal alcohol but she
smokes 20–25 cigarettes per day.
There is no other medical history of
note.
She
lives in a council flat
with her partner
who is also
taking prescribed methadone. She denies any domestic
violence within the relationship.
Examination
The
woman appears thin and anxious.
The blood pressure
is 107/65 mmHg and pulse
90/min. The abdomen is distended with the fundus
palpable at the
umbilicus. The fetal heartbeat is heard with a hand-held
Doppler device.
Questions
·
What other investigations should be arranged?
·
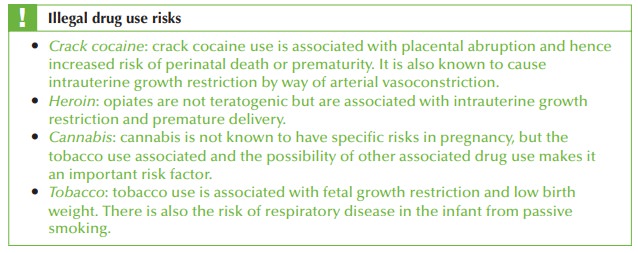
What are the risks
associated with drug use in pregnancy?
·
How
would you manage
this woman during
the pregnancy?
ANSWER
The
woman has been
found to be hepatitis B surface antigen
positive. This needs
further investigation withe antigenicity to determine risk of transmission,
and liver function tests. Assuming the hepatitis B is related
to needle sharing,
she is also at significant risk of hepatitis C and this should also be tested
for at this stage.
A
urine toxicology screen
should be performed with the woman’s
consent, to confirm
the drug history she has given
and what the risks to the fetus
may be.
Management of the pregnancy
Multidisciplinary team
Most units have a specialist team for management of drug-using women
in pregnancy. This should
include specialists in substance misuse,
a social worker,
a specialist midwife and an interested obstetrician.
Opiate replacement
The
woman needs to be encouraged to engage more fully with the methadone replacement programme. This may well mean increasing the methadone regime
to allow her to stop the
street heroin. Once
this has been
achieved then she
can gradually reduce
the dose needed, with appropriate support. It is better
to be still taking a maintenance dose of methadone through the pregnancy than to try and stop
too quickly, resulting in unquantifiable
amounts of illegal drugs being taken during the pregnancy.
Fetal monitoring
The
fetus should be assessed for growth during
the pregnancy in view of the increased risk of intrauterine growth
restriction.
Delivery
Labour should be managed
as for any
non-drug-using woman. The
difference may be that
the usual doses of opiates
needed for analgesia (epidural or systemic) may be insufficient and need to be titrated up to ensure
adequate pain control.
Fetal blood sampling should
be avoided in labour due
to the risk
of vertical transmission of hepatitis B antigen.
Postpartum
The
baby should be administered hepatitis B immunoglobulin at delivery and be given
the accelerated hepatitis B immunization course.
Babies of opiate-using mothers
may have initial
respiratory depression as a result
of the opiates but then
develop withdrawal symptoms. They need immediate transfer to the neonatal unit for management of the symptoms, with reducing doses
of opiates.
Issues of care for the baby should be established between
the social services, medical team and the
parents, prior to delivery.
Related Topics