Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Antenatal Screening
ANTENATAL SCREENING
History
A
31-year-old pregnant Russian
woman came to the UK 6 weeks
ago with her
English husband. As a result she booked late with the midwife at 31 weeks’ gestation. This is her first ongoing pregnancy, having
had two uncomplicated surgical terminations approxi- mately 10 years
ago. She reports
a history of genital herpes
diagnosed by her general
practitioner several weeks
ago. There is no relevant
previous general medical
history or family history.
She
had an apparently normal first-trimester scan in Russia
before arriving in the UK and
has had a normal anomaly
scan in this hospital at 30 weeks’
gestation.
Examination
Blood pressure is normal
and symphysiofundal height
is consistent with
menstrual dates.
Questions
·
What is the diagnosis?
·
How
should the woman
be further investigated and treated?
ANSWER
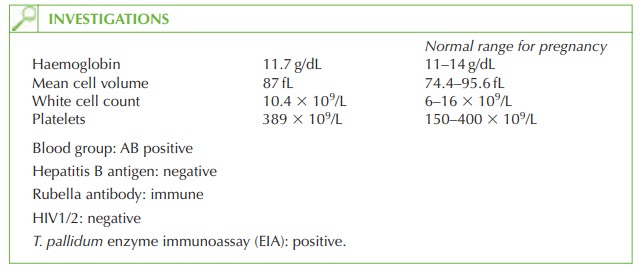
Screening for syphilis is recommended for
all pregnant women
and T. pallidum EIA is a
specific test for syphilis infection. The prevalence of infection is up to 0.3/1000 pregnant women in the UK.
EIA tests that
detect immunoglobulin G (IgG) or IgG and
IgM, T. pal- lidum haemagglutination test and the fluorescent
treponemal antibody-absorbed test (FTA-abs)
are used generally for screening in pregnancy, as they are 98 per cent sensitive and over 99 per cent specific.
In cases with a positive screening
test a second treponemal-specific confirmatory
test should be sent to confirm
the diagnosis. Caution
is needed as treponemal-specific tests cannot differentiate syphilis from other treponemal disease (yaws, pinta
and bejel).
The
diagnosis in this woman is syphilis infection. She should be referred to a genito- urinary medicine clinic for
urgent assessment and
treatment. She may
have a genital
ulcer (possibly misdiagnosed as herpes simplex
by her doctor)
or features of secondary syphilis, but many women diagnosed are asymptomatic (latent
syphilis).
Management
Treatment is with intramuscular penicillin daily for
10 days (doxycycline or erythromycin
if penicillin allergic). Follow-up with a quantitative test
(such as venereal disease research
laboratory [VDRL] should be used to confirm
effective treatment and to monitor
for reinfection. The woman’s
partner should be referred to the genitourinary medicine clinic for testing
(45–60 per cent of partners
will be infected).
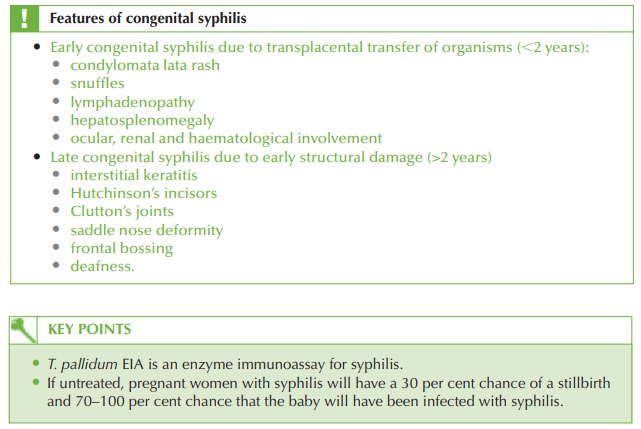
The
paediatricians should be informed
at delivery to assess for signs of early congenital
syphilis (usually
developing in the first few
weeks of life)
and to arrange serological testing.
Untreated, 70–100 per
cent of babies
of mothers with
syphilis infection will
develop con- genital syphilis, with a 30 per cent stillbirth rate.
Related Topics