Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Anti-D
ANTI-D
History
A
couple attends the obstetric clinic
at 20 weeks’ gestation. This is the woman’s fourth pregnancy and second child.
She is 27 years old.
She had a spontaneous vaginal
delivery 4 years ago and this was followed
by two miscarriages, the first
at 8 weeks and the sec-
ond at 14 weeks, for which no cause was identified.
In
this pregnancy she has been generally well except for severe hyperemesis which has now resolved. Her 11–14-week scan confirmed her menstrual dates
and she was given a risk
of Down’s syndrome from her nuchal
test of 1 in 2543.
Her anomaly scan
has just been performed
and shows no fetal abnormalities, and normal fetal growth and liquor
volume.
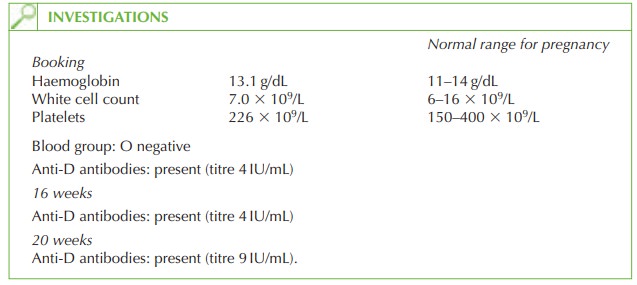
She is known to be Rhesus negative
and her booking and subsequent haematological blood tests are as shown.
Questions
·
What is the diagnosis?
·
What are the potential
consequences of this problem?
·
How
would you further
manage the pregnancy?
ANSWER
The
diagnosis is Rhesus
sensitization as the serum anti-D
titre is increasing, suggesting that sometime exposure
to Rhesus positive
cells has sensitized her, causing her to produce an immune response (anti-D). This may have occurred if she was not given
anti-D at the time of a previous pregnancy.
Consequences
Immunoglobulin G (IgG) anti-D
antibodies cross the placenta and attack fetal
Rhesus- positive red cells.
This causes fetal
haemolysis (haemolytic disease
of the newborn
or the fetus) manifesting as fetal anaemia,
with subsequent fetal
hydrops (excessive accumula- tion of extravascular fluid
e.g. peritoneal, pleural,
pericardial). Intrauterine death
may occur if the
anaemia is not
treated. In milder
cases, the baby
may be severely jaundiced at
delivery, which may
result in neurological impairment. For the
mother there is a potential difficulty crossmatching blood should she have a haemorrhagic complication and need transfusion, due to the presence of the antibodies.
Management
The maternal antibody level should
be monitored two weekly. If the titre exceeds 15 IU/mL, fetal ultrasound should be performed to assess for
growth retardation, signs
of hydrops and liquor
volume. Cordocentesis (sampling fetal blood by ultrasound-guided
aspiration from the
umbilical cord) is needed to determine haemoglobin and to facilitate fetal blood transfusion. If the antibody
titre does not increase further
then ultrasound observation is
likely to be sufficient.
In
this case, the antibody titre
was 15 IU/mL 2 weeks
later and the fetus required
three in utero transfusions during the pregnancy, with delivery by Caesarean section
at 36 weeks.
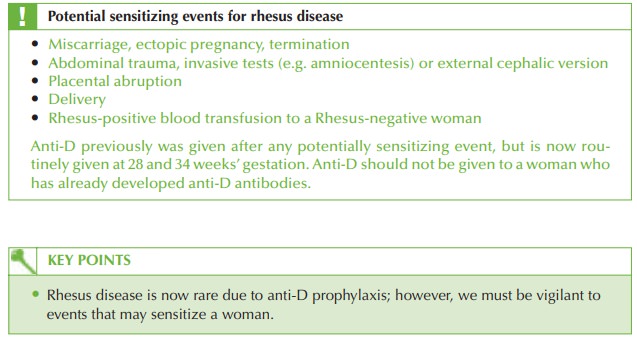
Fifteen per cent of women are Rhesus negative, but due to anti-D prophylaxis, the inci- dence of
Rhesus disease is now very low.
Related Topics