Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Valvular Heart Disease: General Evaluation of Patients
Valvular Heart Disease
1. General Evaluation of Patients
Regardless of the lesion or its cause,
preoperative evaluation should be primarily concerned with determining the
identity and severity of the lesion and its hemodynamic significance, residual
ven-tricular function, and the presence of any secondary effects on pulmonary,
renal, and hepatic function.
Concomitant CAD should not be
overlooked, par-ticularly in older patients and those with known risk factors
(see above). Myocardial ischemia may also occur in the absence of significant
coronary occlusion in patients with severe aortic stenosis or regurgitation.
History
The preanesthesia history should focus
on symptoms related to decreased ventricular function. Symptoms and signs
should be correlated with laboratory data. Questions should evaluate exercise
tolerance, fatiga-bility, and pedal edema and shortness of breath in general
(dyspnea), when lying flat (orthopnea), or at night (paroxysmal nocturnal
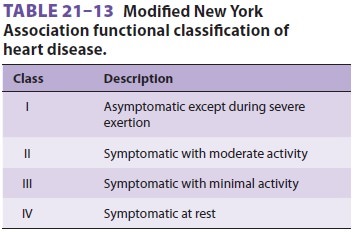
dyspnea). The New York Heart Association functional classification of heart
disease (Table
21–13) is useful for grading the severity of heart failure symptoms
and estimating prognosis. Patients should also be questioned about chest pains
and neurological symptoms. Some val-vular lesions are associated with thromboembolic
phenomena. Prior procedures, such as valvotomy or valve replacement and their
effects, should also be well documented.
A review of medications should evaluate
effi-cacy and exclude serious side effects. Commonly used agents include
diuretics, vasodilators, ACE inhibitors, β-blockers, antiarrhythmics, and
anti-coagulants. Preoperative vasodilator therapy may be used to decrease
preload, afterload, or both. Excessive vasodilatation worsens exercise
tolerance and is often first manifested as postural (orthostatic) hypotension.
Physical Examination
The most important signs to identify on
physical examination are those of congestive heart failure. Left-sided (S3 gallop or pulmonary rales) and right-sided (jugular
venous distention, hepatojugular reflux, hepatosplenomegaly, or pedal edema)
signs may be present. Auscultatory findings may confirm the valvular
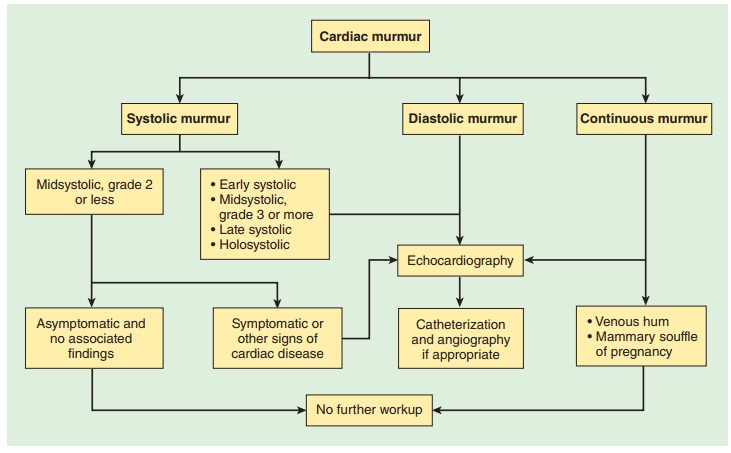
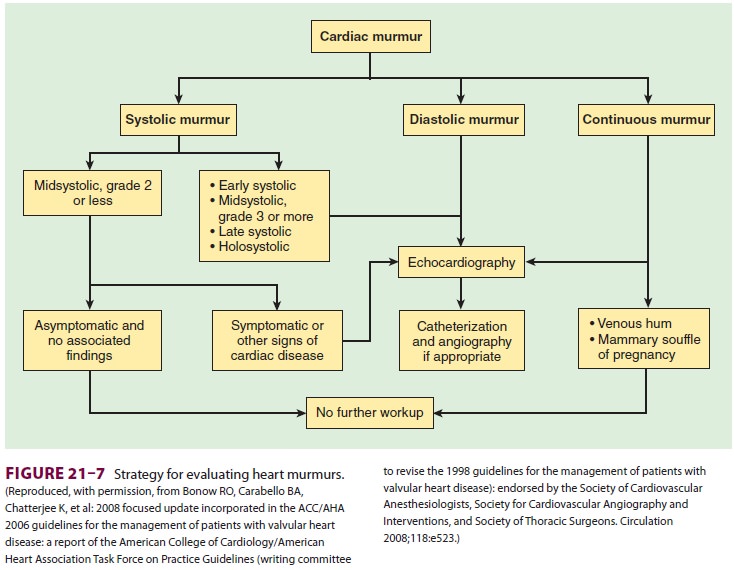
dysfunction ( Figure
21–7), but echocar-diographic studies are more reliable.
Neurological deficits, usually secondary to embolic phenomena, should be
documented.
Laboratory Evaluation
In addition to the laboratory studies
discussed for patients with hypertension and CAD, liver function tests may be
useful in assessing hepatic dysfunction caused by passive hepatic congestion in
patients with severe or chronic right-sided failure. Arterial blood gases can
be measured in patients with significant pulmonary symptoms. Reversal of
warfarin or hepa-rin should be documented with a prothrombin time and
international normalized ratio (INR) or partial thromboplastin time,
respectively, prior to surgery.
Electrocardiographic findings are
generally nonspecific. The chest radiograph is useful to assess cardiac size
and pulmonary vascular congestion.
Special Studies
Echocardiography, imaging studies, and
cardiac catheterization provide important diagnostic and prognostic information
about valvular lesions, but should only be obtained if the results will change
therapy or outcomes. More than one valvular lesion is often found. In many
instances, noninvasive stud-ies obviate the need for cardiac catheterization,
unless there are concerns about CAD. Information from these studies is best
reviewed with a cardiolo-gist. The following questions must be answered:
·
Which
valvular abnormality is most important hemodynamically?
·
What
is the severity of an identified lesion?
·
What
degree of ventricular impairment is present?
·
What
is the hemodynamic significance of other identified abnormalities?
· Is there any evidence of CAD?
The ACC/AHA have prepared detailed
guide-lines to assist in the management of the patient with valvular heart
disease. Although the evaluation of the patient with a heart murmur generally
rests with the cardiologist, anesthesia providers will on occa-sion discover
the presence of a previously undetected murmur on preanesthetic examination. In
particu-lar, anesthetists are concerned that undiagnosed, critical aortic
stenosis might be present, which could potentially lead to hemodynamic collapse
with either regional or general anesthesia. In the past, most val-vular heart
diseases were a consequence of rheumatic heart disease; however, with an aging
surgical popu-lation, increasing numbers of patients have degener-ative valve
problems. More than one in eight patients older than age 75 years may manifest
at least one form of moderate to severe valvular heart disease.
A study conducted in the Netherlands
reported that the prevalence of aortic stenosis was 2.4% in patients older than
age 60 years who were scheduled for elective surgery. Underdiagnosed valvular
disease is particularly prevalent in elderly females.
According to the ACC/AHA guidelines,
auscul-tation of the heart is the most widely used method to detect valvular
heart disease. Murmurs occur as a consequence of the accelerated blood flow
through narrowed openings in stenotic and regurgitant lesions. Although
systolic murmurs may be related to increased blood flow velocity, the ACC/AHA
guide-lines note that all diastolic and continuous murmurs reflect pathology.
Other than murmurs that are thought to be innocent, such as mid-systolic flow
murmurs (grade 2 or softer), the ACC/AHA guide-lines recommend
echocardiographic evaluation.
When new murmurs are detected in a
preoperative evaluation, consultation with the patient’s personal physician is
helpful to determine the need for echo-cardiographic evaluation. In many
centers, immedi-ate echocardiographic evaluation can be performed in the
preoperative area.
Related Topics