Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Cardiovascular Disease
Hypertension: Intraoperative Management
INTRAOPERATIVE MANAGEMENT
Objectives
The overall anesthetic plan for a
hypertensive patient is to maintain an appropriate stable blood pressure range.
Patients with borderline hypertension may be treated as normotensive patients.
Those with long-standing or poorly controlled hypertension, how-ever, have
altered autoregulation of cerebral blood flow; higher than normal mean blood
pressures may be required to maintain adequate cerebral blood flow. Because
most patients with long-standing hypertension are assumed to have some element
of CAD and cardiac hypertrophy, excessive blood pressure elevations are
undesirable. Hypertension, particularly in association with tachycardia, can
precipitate or exacerbate myocardial ischemia, ventricular dysfunction, or
both. Arterial blood pressure should generally be kept within 20% of
preoperative levels. If marked hypertension (>180/ 120 mm Hg) is present preoperatively, arterial
blood pressure should be maintained in the high-normal range (150–140/90–80 mm
Hg).
Monitoring
Most hypertensive patients do not
require special intraoperative monitors. Direct intraarterial pres-sure
monitoring should be reserved for patients with wide swings in blood pressure
and those undergo-ing major surgical procedures associated with rapid or marked
changes in cardiac preload or afterload.
Electrocardiographic monitoring should
focus on detecting signs of ischemia. Urinary output should generally be
monitored with an indwelling urinary catheter in patients with a preexisting
renal impair-ment who are undergoing procedures expected to last more than 2
hr. When invasive hemodynamic monitoring is used, reduced ventricular
compli-ance is often apparent in
patients with ventricular hypertrophy; these patients may require more
intravenous fluid to produce a higher filling pressure to maintain adequate
left ventricular end-diastolic volume and cardiac output. Volume administration
in patients with decreased ventricu-lar compliance can also result in elevated
pulmonary arterial pressures and pulmonary congestion.
Induction
Induction of anesthesia and endotracheal
intubation are often associated with hemodynamic instability in hypertensive
patients. Regardless of the level of preoperative blood pressure control,
manypatients with hypertension display an accentuated hypotensive response to
induction of anesthesia, fol-lowed by an exaggerated hypertensive response to
intubation. Many, if not most, antihypertensive agents and general anesthetics
are vasodilators, cardiac depressants, or both. In addition, many hypertensive
patients present for surgery in a volume-depleted state. Sympatholytic agents
attenuate the normal pro-tective circulatory reflexes, reducing sympathetic
tone and enhancing vagal activity.
Up to 25% of hypertensive patients may
exhibit severe hypertension following endotracheal intuba-tion. Prolonged
laryngoscopy should be avoided. Moreover, intubation should generally be
performed under deep anesthesia (provided hypotension can be avoided). One of
several techniques may be used before intubation to attenuate the hypertensive
response:
·
Deepening
anesthesia with a potent volatile agent
·
Administering
a bolus of an opioid (fentanyl, 2.5–5 mcg/kg; alfentanil, 15–25 mcg/kg;
sufentanil, 0.5–1.0 mcg/kg; or remifentanil, 0.5–1 mcg/kg).
·
Administering
lidocaine, 1.5 mg/kg intravenously, intratracheally, or topically in the airway
·
Achieving
β-adrenergic blockade with esmolol, 0.3–1.5 mg/kg;
metoprolol 1–5 mg;or labetalol, 5–20 mg.
Choice of Anesthetic Agents
A. Induction Agents
The superiority of any one agent or
technique over another has not been established. Propofol, barbi-turates,
benzodiazepines, and etomidate are equally safe for inducing general anesthesia
in most hyper-tensive patients. Ketamine by itself can precipitate marked
hypertension; however, it is almost never used as a single agent. When
administered with a small dose of another agent, such as a benzodiaz-epine or
propofol, ketamine’s sympathetic stimulat-ing properties can be blunted or
eliminated.
B. Maintenance Agents
Anesthesia may be safely continued with
volatile agents (alone or with nitrous oxide), a balanced technique (opioid + nitrous oxide + muscle
relax-ant), or a total intravenous technique. Regardless of the primary
maintenance technique, addition of a volatile agent or intravenous vasodilator
gener-ally allows convenient intraoperative blood pressure control.
C. Muscle Relaxants
With the possible exception of large
bolus doses of pancuronium, any muscle relaxant can be used.
Pancuronium-induced vagal blockade and neu-ral release of catecholamines could
exacerbate hypertension in poorly controlled patients, but, if given slowly, in
small increments, pancuronium is unlikely to cause medically important increases
in heart rate or blood pressure. Moreover, pan-curonium can be useful in
offsetting excessive vagal tone induced by opioids or surgical manipulations.
Hypotension following large (intubating) doses of atracurium may be accentuated
in hypertensive patients.
D. Vasopressors
Hypertensive patients may display an
exagger-ated response to both endogenous catecholamines (from intubation or
surgical stimulation) and exogenously administered sympathetic agonists. If a
vasopressor is necessary to treat excessive hypotension, a small dose of a
direct-acting agent, such as phenylephrine (25–50 mcg), may be use-ful.
Patients taking sympatholytics preoperatively may exhibit a decreased response
to ephedrine. Vasopressin as a bolus or infusion can also be employed to
restore vascular tone in the hypoten-sive patient.
Intraoperative Hypertension
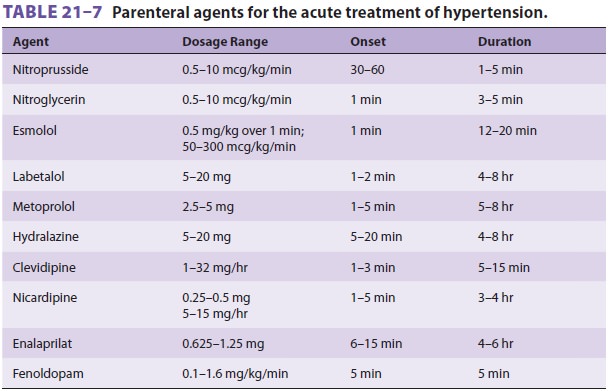
Intraoperative hypertension not
responding to an increase in anesthetic depth (particularly with a vol-atile
agent) can be treated with a variety of parenteral agents (Table 21–7). Readily reversible
causes— such as inadequate anesthetic depth, hypoxemia, or hypercapnia—should
always be excluded before initiating antihypertensive therapy. Selection of a
hypotensive agent depends on the severity, acute-ness, and cause of hypertension;
the baseline ven-tricular function; the heart rate; the presence of
bronchospastic pulmonary disease; and the anes-thetist’s familiarity with each
of the drug options. β-Adrenergic blockade alone or as a
supplement isa good choice for a patient with good ventricular function and an
elevated heart rate, but is relatively contraindicated in a patient with
bronchospastic disease. Metoprolol, esmolol, or labetolol are read-ily used
intraoperatively. Nicardipine or clevidipine may be preferable to β-blockers for
patients with bronchospastic disease. Nitroprusside remains the most rapid and
effective agent for the intraopera-tive treatment of moderate to severe
hypertension. Nitroglycerin may be less effective, but is also use-ful in
treating or preventing myocardial ischemia. Fenoldopam, a dopamine agonist, is
also a useful hypotensive agent; furthermore, it increases renal blood flow.
Hydralazine provides sustained blood pressure control, but also has a delayed
onset and can cause reflex tachycardia. The latter is not seen with labetalol
because of a combined α- and β-adrenergic blockade.
Related Topics